Recap: Treatment Advances in Chronic GVHD
A panel of experts in stem cell transplant and cellular immunotherapy builds a lively discussion on current and emerging treatment options for the management of acute and chronic graft versus host disease.
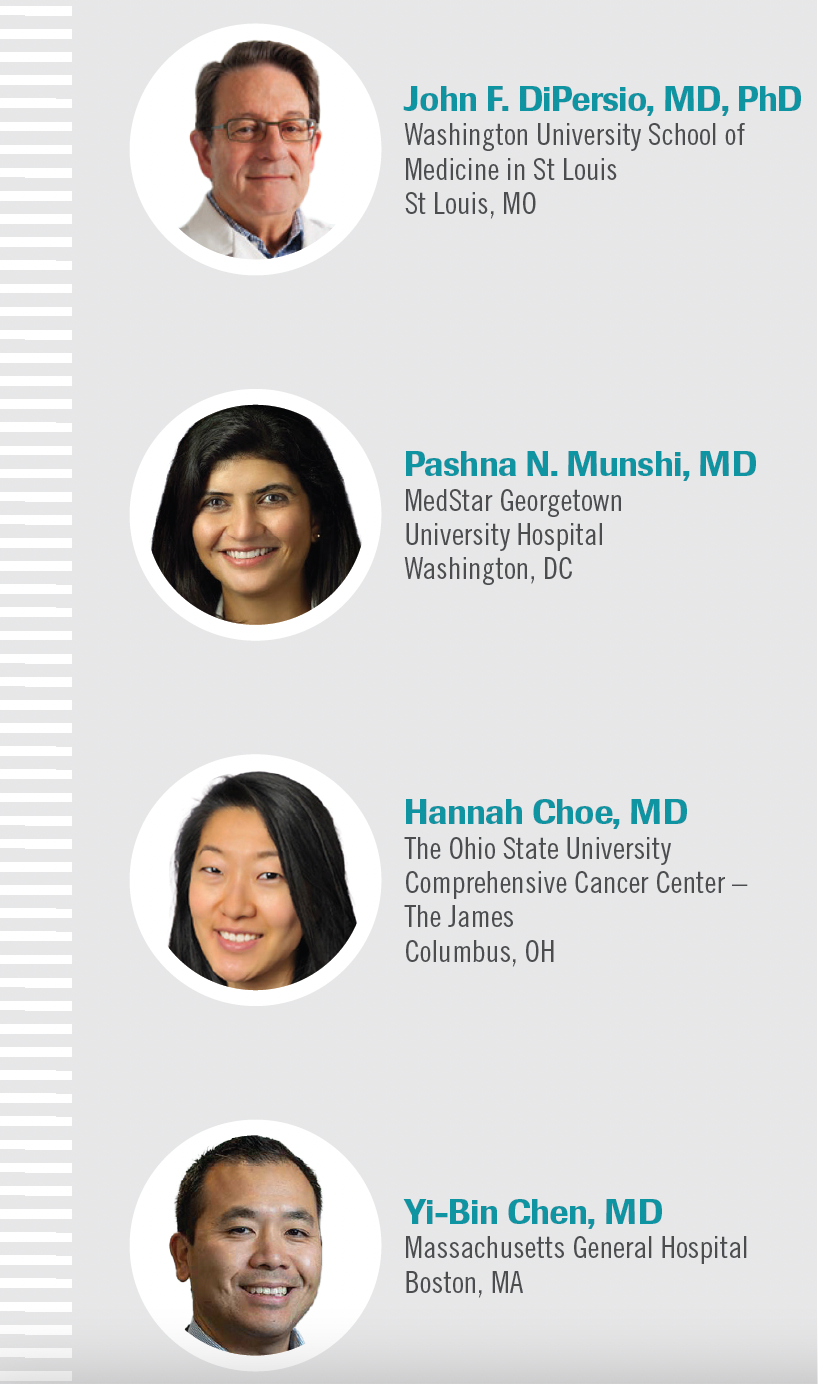
At an Around the Practice program hosted by CancerNetwork®, experts spoke about updates in the treatment of chronic graft-vs-host disease (GVHD). The panel was led by John F. DiPersio, MD, PhD, chief of the Division of Oncology and deputy director of the Alvin J. Siteman Cancer Center at Washington University School of Medicine in St Louis, Missouri.
“Issues with diagnosis and treatment of patients with chronic GVHD…represent, in my humble opinion, some of the most challenging clinical issues that we deal with in the transplantation community,” DiPersio said as a lead-in to the discussion. “We don’t understand that much about the biology of the disease, but we’ve made some progress.”
Other experts on the panel included Pashna N. Munshi, MD, associate clinical director of the Stem Cell Transplant and Cellular Immunotherapy Program at MedStar Georgetown University Hospital in Washington, DC; Hannah Choe, MD, assistant professor and member of the Leukemia Research Program at The Ohio State University Comprehensive Cancer Center – The James in Columbus, Ohio; and Yi-Bin Chen, MD, director of the Hematopoietic Cell Transplant & Cell Therapy Program at Massachusetts General Hospital and associate professor of medicine at Harvard Medical School in Boston.
Acute vs Chronic GVHD
DiPersio: What are the classic signs and symptoms of acute and chronic GVHD?
Chen: We tend to view acute and chronic GVHD as separate diseases. For the most part, they’re separated by their [time to] onset after transplantation and their manifestations. Historically, we had the 100-day mark: acute would occur before it, and chronic would occur after it. That timeline doesn’t matter anymore, it’s much more about the clinical manifestations. There are rare cases where you have patients who have overlapping symptoms of both, but we tend to view acute GVHD as a T-cell–driven immune response.
The organs we think about it affecting include the skin, [with] erythema or red skin rash, and the lower GI [gastrointestinal] tract [which] presents as diarrhea, anorexia, lack of appetite, or persistent nausea. The organ that’s least likely to be involved is the liver, mainly presenting as asymptomatic elevations and liver function tests. Those are the primary organs we look at for acute GVHD.
Chronic [GVHD] is much more indolent; it takes a longer time to develop. Instead of a classic T-cell response, we think there’s a role for B cells, regulatory T cells, and other immunological pathways that are often redundant. The manifestations are no longer this angry rash and diarrhea. They’re more dominated by symptoms we find in classic autoimmune disease: their eyes are dry, the mouth is very dry from lack of salivary production, and there can be ulcerations. The skin is no longer an erythematous rash but looks more like eczema or psoriasis. Almost any organ can be involved. This includes the lungs, the fascia, the underlying connective tissue of the skin, the joints, and the muscles. It’s a very heterogeneous disease which has made progress quite difficult in this chronic GVHD entity.
Munshi: Chronic GVHD is more subtle in my opinion. Sometimes it can creep up on you or your patient; symptoms like oral pain, dry mouth, or taste changes are more apparent. They’ll tell you right away that [their] mouth is burning, things are sensitive, there are ulcers, or that their eyes feel dry. But once the chronic GVHD builds up more in the myofascia and the skin, things like skin tightening—especially if they’re a little overweight—might be missed. Sclerosis could be developing, and they may not know that they have a patch of sclerotic myofascial skin in the abdomen. If you ask them to raise their arm over their head or to get something out of the kitchen drawer, they’ll realize they’re not able to do that anymore. Chronic GVHD is a very subtle phenomenon. As experts, we’re always looking out for it, but many patients may be home with their referring doctors in the community. Things can be missed.
DiPersio: Anytime you’re taking care of a patient late after transplant and something completely odd is going on, always attribute it to chronic GVHD until proved otherwise. It’s almost always true because there are many things that can happen with the joints, fascia, skin, and liver, but also pleural and pericardial effusions.
What’s your sense of the protective effects of acute and chronic GVHD?
Choe:The alloreactivity that causes GVHD, both acute and chronic, is also the alloreactivity that we get the benefit from for graft-vs-leukemia. [Severe GVHD that is not responsive to therapy contributes to] nonrelapse mortality. That’s going to affect survival and quality of life. In the future, [research will focus on how to] differentiate treating GVHD without compromising the risk of relapse.
DiPersio:What about the biology of chronic GVHD compared with acute GVHD?
Munshi: Acute GVHD is a very angry immature immune system. It’s trying to kick at everything it sees. And the main organs that it’s going to affect are the ones that are obviously damaged from previous chemotherapy or radiation conditioning regimen that that patient received. That’s why the lower gut is more vulnerable. In terms of chronic GVHD, it’s more of an autoimmune phenomenon [with a] low level of ongoing, constant cyclical inflammation. Then there is further fibrosis and scarring that eventually takes over, which is very different from the acute loud flare that can happen anytime [during] this chronic inflammatory syndrome.
GVHD Prophylaxis
DiPersio: What are some of the standard prophylaxis regimens for acute and chronic GVHD?
Chen: There are pharmacological-based [interventions and] ex vivo manipulation of the graft, either by positive or negative selection of certain subsets like T cells and so forth. Most of us use pharmacological prophylaxis because it’s less expensive, easier to do, and requires fewer resources and lab expertise. In terms of pharmacological prophylaxis, the long standard has been calcineurin inhibitor–based prevention, being either cyclosporine or tacrolimus paired with a short course of methotrexate post transplant. There have been alternatives involving mycophenolate or sirolimus or adding those to methotrexate as alternatives. With calcineurin inhibitor–based prevention, we generally think the risk of significant acute GVHD is somewhere between 25% and 40% depending on your patient population, and the risk of significant chronic GVHD is probably 40% to 50% depending upon certain specifics of your patient population.
The newest regimen that’s emerging that has been already mentioned is posttransplant cyclophosphamide, [which] is generally paired with tacrolimus and mycophenolate starting on day 5. There have been some regimens using sirolimus in place of tacrolimus as well. Those are the 2 modern backbones of pharmacological prophylaxis. These are 2 regimens that are being compared in ongoing prospective trials with interesting end points to try and figure out what should be the standard of care. I think there are pros and cons of each.
DiPersio: What about the role of abatacept as prophylaxis?
Choe: I’m not as familiar with abatacept. It certainly shows some improvement, but again, the long-term survival benefit [is still unclear]. We’re not using it as standard yet, but it is nice to have an FDA approval for prophylaxis as an option.
DiPersio: In [the GVHD-1 study that led to the approval of abatacept [Orencia]in this setting], the rates of severe acute GVHD were slightly lower. The biggest change was the early infectious-related complications and death. Obviously, the mechanism of how abatacept works as a tolerance-inducing agent is completely different [from] anything else. It’ll be interesting to see if it lasts and stays in our armamentarium, fades away like some things do, or whether we start to complement it by adding other things on top of it to see if we can improve the outcomes.1
CASE
- A 71-year-old man presented following matched unrelated donor hematopoietic stem cell transplant (HSCT) for acute myeloid leukemia (AML).
- He showed successful engraftment at 10 weeks post HSCT.
- Four months post HSCT, the patient experienced grade 2 acute GVHD of the skin.
- He was treated with topical steroids with complete resolution of the rash.
- Sixteen months post HSCT, the patient reported dry eyes and skin rash.
- A physical exam showed a rash with raised areas and patches of thickened skin around 25% of his trunk.
DiPersio: What are your impressions of this patient case? What, if any, GVHD prophylaxis would you have recommended for this patient getting a matched unrelated donor transplant?
Choe: In the absence of a clinical trial, the patient would get our standard of care which currently is tacrolimus/methotrexate. [Because] this patient is over the age of 70, we’re certainly doing reduced-intensity treatment.
Munshi: I’ve been comfortable using posttransplant cyclophosphamide [PTCy] in most of my patients. In the older patients, I like to select for bone marrow graft to mitigate any cytokine release syndrome toxicities; but also, who wants chronic GVHD? We have treatments for it, but it’s best to prevent it. I’ve been very comfortable using PTCy, even in the older patients [with] unrelated donor grafts.
Chen: Our standard of care is [tacrolimus/methotrexate]. It would be for a fully matched donor with reduced-intensity conditioning. It would still be standard tacrolimus/methotrexate outside of a clinical trial, as we await results of the phase 3 BMT CTN 1703/1801 trial [NCT03959241] to see if our standards of care should change.
DiPersio:What do you do for this patient if he developed symptoms of dry eyes and progressive dryness and scaliness of the skin?
Munshi: If you can get away with topical therapy, that’s the best if we can avoid systemic therapy in these patients. But once you have 2 or more organs
involvement, eventually you’ll need to start them on some form of systemic therapy. Of course, if it’s just a simple red rash, if it’s mild, [it involves] probably less than 50% of body surface area. If it continues to progress, we have to think of adding oral steroids.
DiPersio: Let’s say the patient is improving slightly but then progresses again. What’s your next step?
Choe: We try to get these patients in clinical trials to get them the best option. Most trials right now are in the first refractory setting, so we tend to go to the FDA-approved drugs. This would generally be ruxolitinib [Jakafi] or belumosudil [Rezurock] depending on cost, availability, and tolerance. We’re using ruxolitinib in first-line, first year–refractory chronic GVHD and then evaluating for response regularly and evaluating for second-line therapy initiation.
DiPersio: What are you doing for this patient who progresses after a month of steroid therapy?
Chen: Our standard is ruxolitinib. Certainly, we have found that to be the most efficacious and most tolerable option. We have a very low threshold to add ruxolitinib these days. What’s interesting is that the definition of steroid-
refractory chronic GVHD is like shades of gray. For many of my patients, they may qualify with a partial response to steroids but it’s not satisfactory [enough to either of us]. I have a very low threshold to move on from steroids and use ruxolitinib as our standard second-line agent.
DiPersio: We have 3 drugs that are approved for chronic GVHD: ibrutinib [Imbruvica], [belumosudil], and ruxolitinib. The first 2 drugs were approved with single-arm, open-label small studies. Then the only randomized trial is the ruxolitinib study. I would say that because it’s so hard to measure responses; sometimes the responses are meaningful, but many times they are hard to measure.
The ruxolitinib study [REACH3 (NCT03112603)] was against the standard of care, best available therapy.2 If you really want to know if a drug is effective, you have to test it in a randomized prospective trial.
CASE Continued
- The patient responded to prednisone and was tapered off after 3 months.
- He was followed up every
2 months. - At 22 months post HSCT, the patient reported muscle and joint pain, which was making it difficult to take his daily walks.
DiPersio:What are you thinking of giving this patient at this point?
Choe: Belumosudil has been shown to lead to response in patients who have failed ruxolitinib in a phase 2 trial [NCT03640481]. It’s certainly an option. Belumosudil is currently going through what ruxolitinib was going through when it was first FDA approved, which is delays in being able to start it because of insurance issues and access and cost. Eventually, it might be a more readily available option. What we do at our center right now is for patients who are refractory to ruxolitinib is to get them into a clinical trial and evaluate what the cost to the patient would be to try to do belumosudil. If belumosudil is an option and a clinical trial is not, then we’ll start belumosudil and monitor for tolerance, then have a low threshold to go to clinical trial.
DiPersio: In these trials, the major effect has been to reduce progression. There have been very few studies that show major responses, especially in the key organ systems, but it’s the time to progression that seems to be the main thing. What are the expectations for someone who has severe chronic GVHD that goes on a new medication?
Choe: The overall response rate is relatively high for these new agents, but the complete response rate remains very low. Complete response is in all organ systems involved, so that might be asking for too much with current therapies. It is something we’re hoping for in future clinical trials. For me, the biggest thing is how quickly can I get them on a lower dose of steroids? How much can I preserve of their functional capacity and their tolerance off steroids? If we’re able to stabilize or improve symptoms to a partial response and I’m able to wean [them off] steroids more quickly, that’s certainly a win.
Chen: This illustrates that we need some better diagnostics to understand what pathways are active in which patient. Most of our patients who are significantly affected do end up on multiple therapies. If you look at the trials today that have been mentioned and the end points that we’ve used, greater than 90% of those responses are all PRs [partial responses]. There are few CRs and that may be inherent to the disease; maybe we don’t have the right drugs. It also may be that we don’t understand what pathways are driving the disease itself. We need more therapies, to understand how to use them, and precision medicine–based approaches to be able to understand what therapies are best for which patient. If we had those tools, we would go a long way here.
DiPersio: What about B-cell therapies like ibrutinib, low-dose IL-2 for
enhancing [T-regulatory cell] production, and rituximab [Rituxan]? Is anybody considering these or are these fourth-line therapies?
Choe: I’m concerned about the infection risk and hypogammaglobulinemia. But yes, I’m sure there is a role for rituximab and IL-2. Of course, I haven’t seen that used. Even as a fellow, I haven’t had experience using that, so I actually would ask you what you think IL-2 therapies do to our patients in this era of approvals. But I haven’t challenged chronic GVHD with rituximab and B-cell therapies.
Chen: I’ve personally found ibrutinib is difficult to use. The data published in the real-world experience back that up3 [and the supporting data for the approval are from] single-arm, small sample–size trials where there’s a huge bias in a disease [for which judging] response is very subjective. The real-world experience would suggest the efficacy really isn’t all that significant and there’s a good amount of toxicity from using ibrutinib, not just the B-cell depletion and hypogammaglobulinemia but also cardiac to GI toxicities and muscle cramps.
DiPersio: What are you doing for patients who are out a year or 2 from grafting but develop chronic GVHD on low levels of immunosuppression [due to] COVID-19? Are you vaccinating and watching them, are you vaccinating them and watching their anti-COVID spike protein antibody titers, or are you actually giving them Evusheld (AZD7442)?
Munshi:In our program, we decided that all our patients who were immunocompromised, whether they’re within 100 days or out 1 to 2 years, are getting the Evusheld protection. Obviously, if they have chronic GVHD, we hope that they’ve already been vaccinated and had their booster. Then we are checking the spike protein level in their body for antibody response.
Chen: We don’t have an organized algorithm partly because it’s such a
rapidly changing environment. In general, I worry about long-term chronic GVHD more than any other transplant population because most of our patients are now receiving grafts from vaccinated donors. There’s some adaptive immunity that’s transferred, whereas patients with chronic GVHD who [received a transplant] years ago never had any immunity against COVID-19. If they’re on immunosuppression like the drugs we listed, they certainly have an impaired ability to respond. I worry about them the most. Thankfully, the strains present right now seem to have become less severe and that’s been helpful. But from an immunity perspective, we obviously recommend vaccination, but [we’ve] seen flares of chronic GVHD that can happen…with any vaccine. We do give Evusheld, then we measure the spike antibodies, and then we have trials coming up using other monoclonal antibody products. It’s unfortunate because we don’t have an organized treatment algorithm, but that’s also because of how fast this is changing.
Choe: We hinge everything on vaccination regardless of the immunosuppression, …understanding that ruxolitinib and other immunosuppressants we’re using limit the patient’s ability to mount a response. We’re still giving 3 full doses plus a booster. Shortly, we’re going to be giving another booster once the FDA approves it. In certain cases, depending on patient history, [we’re also] considering Evusheld. We are not broadly using Evusheld for the same reason that everyone just mentioned as we are not sure about the efficacy with current and future strains.
References
- FDA approves abatacept for prophylaxis of acute graft versus host disease. FDA. December 15, 2022. Accessed April 15, 2022. https://bit.ly/3voEyJB
- Zeiser R, Polverelli N, Ram R, et al; REACH3 Investigators. Ruxolitinib for glucocorticoid-refractory chronic graft-versus-host disease. N Engl J Med. 2021;385(3):228-238. doi:10.1056/NEJMoa2033122
- Chin KK, Kim HT, Inyang EA, et al. Ibrutinib in steroid-refractory chronic graft-versus-host disease, a single-center experience. Transplant Cell Ther. 2021;27(12):990.e1-990.e7. doi:10.1016/j.jtct.2021.08.017
EP: 1.Defining Acute and Chronic GVHD: Signs and Symptoms
EP: 2.Impact of GVHD on Leukemic Relapse and Patient Outcomes
EP: 3.Differences in Pathology of Acute and Chronic GVHD
EP: 4.Chronic GVHD Risk Factors and Prevention
EP: 5.Counseling Patients on the Long-Term Management of GVHD
EP: 6.The Role of Prophylaxis Regimens for GVHD
EP: 7.Clinical Scenario 1: First- and Second-Line Treatment for GVHD
EP: 8.The Effect of Trial Design on Approval of GVHD Therapies
EP: 9.Clinical Scenario 2: Steroid-Refractory Chronic GVHD
EP: 10.The Role of Photopheresis for GVHD Following Progression
EP: 11.Additional Approaches for Steroid-Refractory Chronic GVHD
EP: 12.Treatment Approaches Using Ruxolitinib in GVHD
EP: 13.Recap: Treatment Advances in Chronic GVHD
EP: 14.Perspectives on COVID-19 Prophylaxis and Vaccination
Oncology Peer Review On-The-Go: Minority Treatment Disparities and Clinical Trial Enrollment
July 6th 2020The first episode of CancerNetwork's podcast Oncology Peer Review On-The-Go explores disparities in cancer care treatment among minorities and the significance of a representative sample in clinical trials.