New Paradigm Emerging in Prostate Cancer, Moving Chemo Up the Line
The STAMPEDE trial suggests that survival can be improved in metastatic prostate cancer patients with the addition of docetaxel to frontline hormonal therapy.
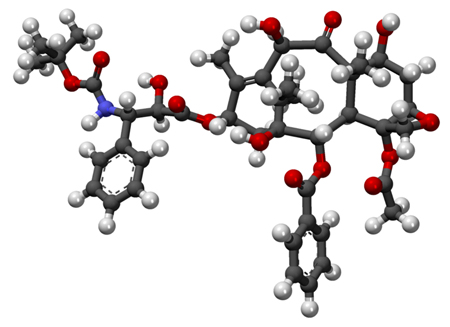
3D ball-and-stick model of docetaxel
A new large clinical trial suggests that survival can be improved in men with metastatic prostate cancer with the addition of docetaxel chemotherapy to frontline hormonal therapy. Treatment-naive men with advanced prostate cancer who received both docetaxel and hormonal therapy lived an average of 10 months longer compared with men who were treated with hormonal therapy alone.
After a median follow-up of 42 months, overall survival improved by 24% in the docetaxel arm (77 months) compared with the standard of care (SOC) arm (67 months).
Docetaxel also extended time to relapse by 38% in all patients.
The results were presented by study author Nicholas David James, MD, PhD, director of the cancer research unit at the University of Warwick and consultant in clinical oncology at Queen Elizabeth Hospital Birmingham in the United Kingdom, at the presscast ahead of the 2015 American Society of Clinical Oncology (ASCO) Annual Meeting.
“The bias has been to use hormonal therapy until it is exhausted and then at the last moment to use chemotherapy, which is often a self-defeating strategy,” said ASCO President Peter Paul Yu, MD, FACP, FASCO.
Following last year’s ASCO plenary session results, which indicated that this may be the wrong strategy, this larger study adds evidence that the addition of chemotherapy early in the course of treatment may be paradigm-shifting, commented Yu.
The current study, Systemic Therapy in Advancing or Metastatic Prostate Cancer: Evaluation of Drug Efficacy (STAMPEDE), is the largest randomized study in men with prostate cancer to date, with more than 6,500 men recruited since 2005. This ongoing UK-coordinated study can be adapted to add new therapies or to change the SOC in this rapidly evolving cancer population.
The currently reported data from STAMPEDE included 2,962 hormone-naive prostate cancer patients assigned to one of four therapies: SOC with androgen deprivation therapy for at least 3 years and radiation therapy for eligible patients; SOC with 6 cycles of docetaxel; SOC with zoledronic acid for 2 years; and SOC with both docetaxel and zoledronic acid.
The addition of zoledronic acid to hormonal therapy, or zoledronic acid to both hormonal therapy and docetaxel did not improve survival compared with SOC plus docetaxel alone.
Men with detectable metastatic disease benefited the most from the addition of docetaxel. Among this subset of patients (60% of the 2,962 included in the analysis), survival improved from 43 months to 65 months in the docetaxel arm.
Docetaxel should be considered routine in men with metastatic prostate cancer, said James during the presscast. Clinicians should also discuss the addition of docetaxel for patients with advanced non-metastatic disease since, according to this study, chemotherapy appears to reduce the risk of relapse. But, longer follow-up is needed to understand the full overall survival advantage in men with non-metastatic disease.
“There is also the hint that this [treatment] strategy of bringing chemo earlier on can have a benefit even in men who don’t have metastases,” said Wu.
Although the addition of docetaxel did cause toxicities in comparison with hormonal therapy alone, these side effects were manageable and caused few discontinuations.
The study authors plan to report the quality-of-life analysis for these patients at a later time.