STORM: Adjuvant Sorafenib Had No Effect on HCC Recurrence
Treatment with sorafenib after curative resection or ablation of hepatocellular carcinoma did not improve recurrence-free survival compared with placebo, according to the results of the phase III STORM trial.
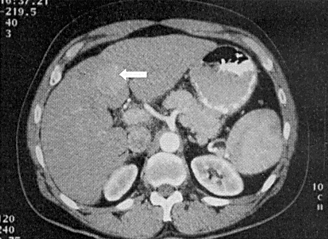
CT of a solitary hepatocellular carcinoma (arrow): arterial phase
Treatment with sorafenib after curative resection or ablation of hepatocellular carcinoma (HCC) did not improve recurrence-free survival compared with placebo, according to the results of the phase III STORM trial (abstract 4006) presented by Jordi Bruix, MD, of the University of Barcelona, at the 2014 American Society of Clinical Oncology (ASCO) Annual Meeting.
“Patients with liver cancer who have undergone treatment expected to provide cure are hampered by high grade of recurrence that can be as high as 70%,” Bruix said during his presentation. “Alternatively there is no effective option that can reduce the incidence of these events. This is an unmet need in these patients.”
The placebo-controlled, double-blind STORM trial was designed to evaluate the efficacy and safety of adjuvant sorafenib in patients with HCC who have no lesions after curative resection or ablation.
The study included patients with HCC who underwent either surgical resection or local ablation. Once proven to have no residual disease, the patients were randomly assigned to 400 mg twice daily sorafenib (n = 556) or placebo (n = 558). The primary endpoint of the analysis was recurrence-free survival.
There was no difference in recurrence-free survival between the two study groups. The median recurrence-free survival was 33.4 months for sorafenib compared with 33.8 months for placebo (HR = 0.94; 95% CI, 0.780-1.134).
A subgroup analysis of recurrence-free survival that looked at age, sex, geographic origin, degree of risk, liver function, treatment received, and etiology showed no difference between the two treatment arms.
The secondary endpoint of the study was time to recurrence. Again, there was no significant difference between the two treatment arms. The median time to recurrence was 38.6 months for sorafenib compared with 35.8 months for placebo (HR = 0.891; 95% CI, 0.735-1.081).
Recurrence-free survival and time to recurrence done by investigator assessment also showed no difference between the treatment arms. Additionally, an overall survival analysis showed about 75% survival in both arms with no significant difference yet between the two treatments.
Safety of the drug was analyzed in all patients who had at least one dose of the study drug. There were more drug-related adverse events in sorafenib arm (94.1% vs 46.4%).
“About 30% of patients in the sorafenib arm had discontinued treatment at 3 months, and almost half by 1 year,” Bruix said. “This translated into a shorter treatment duration in and a lower actual daily dose in the sorafenib arm as compared with the placebo arm.”