Judd W. Moul, MD, spoke with CancerNetwork® about the latest research from the journal ONCOLOGY® on the treatment of a patients with evidence of prostate cancer despite multiple negative prognostic tests.

Your AI-Trained Oncology Knowledge Connection!

Judd W. Moul, MD, spoke with CancerNetwork® about the latest research from the journal ONCOLOGY® on the treatment of a patients with evidence of prostate cancer despite multiple negative prognostic tests.
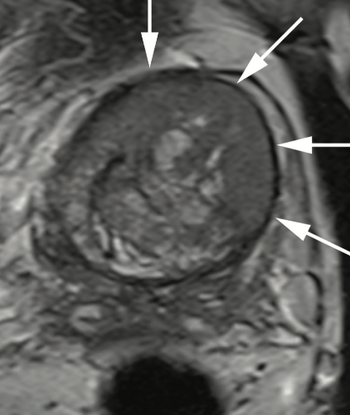
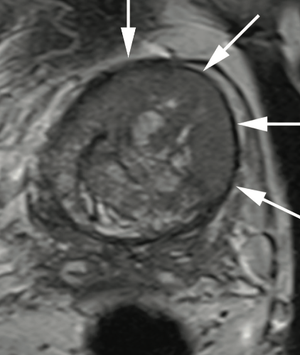
Dr. Judd W. Moul, MD, and colleagues present the case of a man, aged 73 years, with a prostate-specific antigen level of 110 ng/mL after 4 negative prostate biopsies and 4 negative prostate MRIs.

Judd Moul, MD, discusses the gravity of new data on systemic therapies for men with castration-resistant prostate cancer and how they can be of use during the COVID-19 pandemic.

Dr Raoul Concepcion leads a multidisciplinary expert panel in a discussion about the challenges of long-term follow-up of prostate cancer in patients with negative bone/CT but positive molecular indicators of recurrence.
An expert panel discusses the challenges of detecting and managing biochemical recurrence in the context of oligometastatic prostate cancer.

Dr Munir Ghesani reviews and comments on data regarding the sensitivity of imaging modalities in detecting biochemical recurrence in prostate cancer.

Dr Raoul Concepcion leads a panel discussion on a case of a 64-year-old man with multifocal prostate cancer treated with IMRT who refused ADT.

Munir Ghesani, MD, an expert in nuclear medicine, describes the factors that differentiate available tracers and provides guidance on tracer selection.

An expert panel reacts to polling data on choice of imaging modalities for patients with prostate patients after definitive therapy and share their insights about best practices.
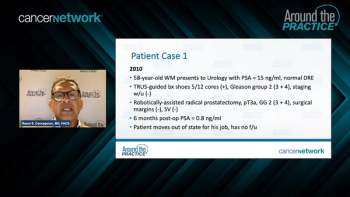
Raoul Concepcion, MD, presents the case of a 58-year-old man who had a radical prostatectomy 6 months prior and discusses how aspects of the case influence treatment selection.

Experts in prostate cancer discuss considerations for initiating ADT therapy after definitive treatment in patients with prostate cancer in the context of biochemical recurrence.

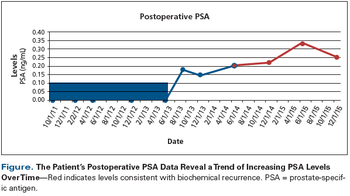
Dr Judd Moul and colleagues discuss best practices for monitoring patients with prostate cancer after definitive therapy.
Dr Raoul Concepcion leads a panel of experts in prostate cancer in setting the stage for case-based discussions of biochemical recurrence.
The Duke Cancer Institute expert discusses the possible impact and ramifications of delays in cancer screening and diagnosis due to the COVID-19 pandemic.

In this video, Dr. Judd Moul discusses disparities in prostate cancer screening among African-American men, and the need for more research in this area.

Most men with clinically important localized prostate cancer deserve first-line open or robotic radical prostatectomy.

Sexual and urinary morbidities resulting from treatment of pelvic malignancies are common. Awareness of these complications is critical in order to properly counsel patients regarding potential side effects and to facilitate prompt diagnosis and management.
A 66-year-old Caucasian man with a history of hypertension, hyperlipidemia, and rheumatoid arthritis was diagnosed with prostate cancer.

This management guide covers the treatment, diagnosis, and staging of prostate cancer.
This article reviews recent evidence suggesting an increased risk of pneumonia, cardiovascular disease, and acute kidney injury in men treated with ADT and consider whether the incidence of such events differs with the treatment modality.

This is an exciting time for physicians who care for patients with advanced prostate cancer, and more importantly a time of heightened optimism for these men and their families.

Of course we should offer active surveillance to African-American men with localized prostate cancer! We simply need to do it selectively and in a smarter way-and we need to be aware of some of the potential pitfalls.

Over the last decade, robotic-assisted laparoscopic prostatectomy (RALP) has rapidly gained in popularity, primarily for three reasons: the enthusiasm of surgeons keen to try something new, medical marketing, and patients’ desire to avoid side effects from surgery.

These are, indeed, exciting times for patients with metastatic prostate cancer and the clinicians who care for them.

As a clinician and researcher in the prostate cancer field, I have been hearing that prostate cancer is “20 years behind” breast cancer now for the last 25 years!

A 36-year-old male with a history of cryptorchidism of the right side, treated with orchidopexy at the age of 4, presented with bilateral testicular swelling. Investigations included laboratory workup, ultrasound of both testes, as well as CT-scan of the chest, abdomen, and pelvis. Initial treatment was bilateral orchiectomy.

Rising prostate-specific antigen (PSA) in nonmetastatic prostate cancer occurs in two main clinical settings: (1) rising PSA to signal failed initial local therapy and (2) rising PSA in the setting of early hormone-refractory prostate cancer prior to documented clinical metastases. Most urologists and radiation oncologists are very familiar with the initial very common clinical scenario, commonly called "biochemical recurrence." In fact, up to 70,000 men each year will have a PSA-only recurrence after failed definitive therapy. The ideal salvage therapy for these men is not clear and includes salvage local therapies and systemic approaches, of which the mainstay is hormonal therapy. Treatment needs to be individualized based upon the patient's risk of progression and the likelihood of success and the risks involved with the therapy. It is unknown how many men per year progress with rising PSA while on hormonal therapy without documented metastases. This rising PSA disease state is sometimes called, "PSA-only hormone-refractory prostate cancer." As in the setting of initial biochemical recurrence, evidence-based treatment options are limited, and taking a risk-stratified approach is justified. In this article, we will explore these prostate cancer disease states with an emphasis on practical, clinically applicable approaches.

In this review, we describe how clinical investigators addressed some of the challenges in prostate cancer chemotherapy trials 20 years ago, and we indicate what has evolved in the field since that time. We consider the impact that prostate-specific antigen measurement had in this setting, evolving clinical paradigms, multidisciplinary programs, and the current armamentarium of cancer treatment, including targeted molecular therapy, for patients with hormone-refractory disease.

There are many characteristics that set the military apart from the general population. But there was one particularly appealing characteristic: It is an equal-access-to-care culture. Of course, in a country as large and diverse as America, we can't expect to replicate the equal-access model of the US military. But we can try.

I am honored and delighted to beable to comment on the outstandingcontribution from Drs. Cooperberg,Park, and Carroll relating recentprostate cancer research fromthe various national efforts in prostatedisease research database efforts.As a former director of the Departmentof Defense Center for ProstateDisease Research (DoD-CPDR), Iwas blessed to be able to lead one ofthese database efforts as well as collaboratewith Dr. Carroll and his colleaguesfrom the Cancer of theProstate Strategic Urologic ResearchEndeavor (CaPSURE). Dr. AnthonyD'Amico and his colleagues headedseveral of our joint collaborationsfrom Harvard. In this light, I wouldlike to focus my editorial commentson providing a more in-depth reviewof work[1] that was briefly mentionedin the article by Cooperberg et al.

Published: April 22nd 2021 | Updated:

Published: April 29th 2021 | Updated:

Published: May 6th 2021 | Updated:

Published: April 15th 2021 | Updated:

Published: April 29th 2021 | Updated:
Published: March 14th 2022 | Updated: