A panel of medical oncologists provides insights on managing toxicities in patients with triple-negative breast cancer who are receiving antibody-drug conjugates.

Your AI-Trained Oncology Knowledge Connection!

A panel of medical oncologists provides insights on managing toxicities in patients with triple-negative breast cancer who are receiving antibody-drug conjugates.
Ruth M. O’Regan, MD, and Anna Weiss, MD, discuss treatment paradigms for patients with metastatic triple-negative breast cancer and the role of surgery.
The expert panel provides clinical insights on treating patients with high-risk or locally advanced triple-negative breast cancer.
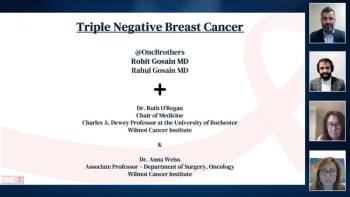
Ruth M. O'Regan, MD, and Anna Weiss, MD, join the Oncology Brothers, Rahul Gosain, MD, and Rohit Gosain, MD, to discuss the treatment of early-stage node-negative triple-negative breast cancer (TNBC).

This video reviews various trials that aimed to improve outcomes or minimize toxicities among patients receiving adjuvant treatment for HER2-positive breast cancer.

Additional insight into the biology of ER-positive breast cancers, particularly the higher risk luminal B cancers, could aid in identifying potential targets and new, effective therapies. And though the majority of triple-negative breast cancers are the “basal-like” subtype, significant proportions are in other subtypes.

As our knowledge of the molecular profiles of breast cancer has increased as a result of moving closer to our goal of individualized therapy, it is clear that we need to re-think our approach to the adjuvant treatment of early-stage breast cancer.

With the advent of aromataseinhibitor use in the adjuvantsetting,[1] and the inceptionof trials examining their usefor breast cancer prevention, it seemsprudent to evaluate what we know todate about the long-term effects of these agents. Unfortunately, unlike selectiveestrogen-receptor modulators(SERMs)-in particular tamoxifen,[2]which has been used for over 15 yearsin patients with early-stage breast cancer-long-term data on the use of aromataseinhibitors are minimal.

The use of aromatase inhibitorshas increased dramatically inthe past few years as a resultof the emergence of new, more specificagents, such as anastrozole(Arimidex), exemestane (Aromasin),and letrozole (Femara). This class ofagents effectively blocks the peripheralformation of estradiol, decreasingits concentration to less than 10%,while maintaining selectivity.[1]Evaluation of these selective aromataseinhibitors as adjuvant therapyfor early-stage breast cancer wasbased on the findings of trials inmetastatic breast cancer, summarizedby Visvanathan and Davidson, thatdemonstrated the equivalence and,in some cases, superiority of thearomatase inhibitors comparedwith megestrol and tamoxifen,including their superior side-effectprofile.[2-4]

Tamoxifen (Nolvadex), a selective estrogen-receptor modulator, or SERM, is currently the endocrine therapy of choice for all stages of hormone-responsive breast cancer. Only tamoxifen has been approved by the US Food and

Published: March 1st 2003 | Updated:

Published: September 1st 2001 | Updated:

Published: March 15th 2013 | Updated:

Published: February 18th 2011 | Updated:

Published: May 1st 2003 | Updated:

Published: January 10th 2018 | Updated: