Prostate Cancer
Latest News
Latest Videos

Podcasts
CME Content
More News

Panelists discuss how, Copper-64 (^64Cu)–labeled PSMA-targeted PET imaging is emerging as a promising modality in prostate cancer diagnosis. The phase 2 SOLAR study (NCT05653856) demonstrated that ^64Cu-PSMA I&T PET/CT effectively detects metastatic prostate cancer, meeting primary end points related to correct localization rates. Compared with gallium-68 (^68Ga) and fluorine-18 (^18F), ^64Cu offers a half-life of approximately 12.7 hours, facilitating centralized production and distribution, which may improve accessibility

A recommendation from an independent data monitoring committee prompted the discontinuation of the phase 3 CAPItello-280 trial.

Data show that patients who undergo grade group 1 prostatectomies may experience an increased likelihood of higher risk features.

BMI, serum albumin, and G8 screening tool scores were all factors correlated with the likelihood of experiencing a grade 3 or higher AE.
Toxicity complications were assessed between single- and multiple-treatment modalities for patients with localized prostate cancer.

Panelists discuss how PSMA PET imaging identified a region of high tracer uptake, guiding medical professionals to implement a focal radiation boost. This approach improved treatment precision and targeting of aggressive areas, highlighting the potential for personalized, effective therapies.

Panelists discuss how PSMA PET imaging has significantly influenced prostate cancer management by enabling precise detection of metastatic lesions, thereby informing and altering treatment strategies. For instance, a study demonstrated that ^68Ga-PSMA-11 PET/CT impacted definitive radiation therapy (RT) planning in 16.5% of patients, leading to modifications in RT fields based on the imaging findings.

Administering 177Lu for mCRPC is a “team sport”, according to Steven Finkelstein, MD, DABR, FACRO.

Panelists discuss how PSMA PET imaging is increasingly utilized to assess treatment response in prostate cancer, offering superior accuracy over PSA monitoring alone. Incorporating PSMA PET into clinical practice involves considering factors such as timing post treatment and the specific clinical scenario. For instance, studies have demonstrated that PSMA PET/CT can detect intraprostatic and metastatic lesions even at very low PSA levels during treatment monitoring.

Panelists discuss how, PSMA PET imaging significantly enhances surgical decision-making in prostate cancer by precisely identifying tumor location, extent, and metastatic spread with superior sensitivity compared to conventional imaging. This molecular targeting enables more accurate surgical planning, improved patient selection for radical prostatectomy versus targeted approaches, and better identification of lymph node involvement, ultimately allowing for personalized treatment strategies that maximize oncological outcomes while minimizing unnecessary interventions.

After the recent approval of 177Lu in PSMA+/mCPRCP prior to chemotherapy, Steven Finkelstein, MD, DABR, FACRO, highlights the importance of this milestone.

Steven Finkelstein, MD, DABR, FACRO, spoke about the impact of the approval of 177Lu for patients with PSMA-positive mCRPC.

Results from the KEYNOTE-921 trial demonstrated that pembrolizumab with docetaxel did not elicit efficacy improvements vs placebo with docetaxel in prostate cancer.

Prolaris in Practice: Guiding ADT Benefits, Clinical Application, and Expert Insights From ACRO 2025
Steven E. Finkelstein, MD, DABR, FACRO discuses how Prolaris distinguishes itself from other genomic biomarker platforms by providing uniquely actionable clinical information that quantifies the absolute benefit of androgen deprivation therapy when added to radiation therapy, offering clinicians a more precise tool for personalizing prostate cancer treatment strategies.

Alvaro Martinez, MD discusses how emerging genomic risk stratification tools such as the clinical cell-cycle risk (CCR) score are transforming personalized prostate cancer treatment by enabling more nuanced assessments of metastasis risk and treatment intensification strategies beyond traditional NCCN risk groupings.

Daniel Kim, MD, MBA discusses how genomic testing has revolutionized patient selection for active surveillance by integrating molecular insights that transcend traditional clinical parameters, enabling more nuanced risk stratification and personalized management of intermediate-risk prostate cancer.

Dwight E. Heron, MD, MBA, FACRO, FACR discusses how advanced multi-omics approaches, personalized precision medicine techniques, artificial intelligence–driven genetic interpretation tools, and emerging gene editing technologies such as CRISPR (clustered regularly interspaced short palindromic repeats) are poised to revolutionize clinical practice by enabling more targeted diagnostics, predictive risk assessments, and individualized treatment strategies across oncology, rare disease management, and chronic condition prevention.

Christopher Lee, MD discusses how genomic biomarker testing has revolutionized prostate cancer management by enabling a precision medicine approach that transitions from population-based treatments to individualized therapeutic strategies based on precise molecular profiling.
Multidisciplinary collaboration may help in minimizing the treatment burden among patients with prostate cancer, according to Curtiland Deville Jr, MD.

Panelists discuss how PSMA PET imaging plays a crucial role in detecting biochemical recurrence of prostate cancer, offering superior sensitivity and specificity compared with conventional imaging methods. In clinical practice, PSMA PET is typically ordered when there is a rise in prostate-specific antigen (PSA) levels post treatment, indicating potential recurrence. The imaging results significantly influence treatment decisions such as distinguishing between localized salvage therapy and systemic treatments. Pivotal trials have demonstrated the efficacy of various tracers.

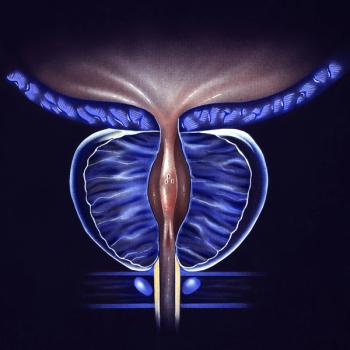
Panelists discuss how PSMA PET imaging plays a crucial role in the initial staging of prostate cancer, offering superior accuracy over conventional methods. Medical professionals consider factors such as diagnostic performance, tracer availability, and patient-specific characteristics when selecting appropriate PSMA PET agents. The integration of PSMA PET findings into clinical practice has led to more precise treatment planning, potentially improving patient outcomes. Pivotal trials have demonstrated the efficacy of various PSMA PET tracers in detecting prostate cancer metastases.

The phase 3 MIRAGE trial findings show that PROSTOX ultra was validated as a biomarker to predict genitourinary toxicity following SBRT.
Focused, high-dose radiotherapy doses may prolong survival and the interval to subsequent therapy for patients with advanced prostate cancer.
Data show increasing use of proton therapy overall but widening gaps in populations who have access to this treatment, Curtiland Deville Jr, MD, says.

Panelists discuss how high-quality imaging is crucial for accurately staging prostate cancer, guiding treatment decisions, and optimizing patient outcomes. Superior resolution and sensitivity of PSMA PET tracers enhance lesion detection, influencing surgical, radiation, and systemic therapy choices. Differences in tracer properties impact specificity, affecting treatment planning. Advanced imaging reduces uncertainty, improving risk stratification and therapeutic precision.