Mucosal melanoma is a rare disease that is distinct from melanomas arising at other sites in the body. While melanocytes are most abundant in the skin, they can be found in smaller numbers in the mucous membranes, as well as in the eye. There are epidemiologic, genetic, and other physiologic differences between melanomas arising from melanocytes at these various sites, and these differences have important implications for both disease prognosis and treatment. Here, we review the features of mucosal melanoma that distinguish it from melanomas arising at other sites, and we highlight recent biological discoveries and emerging treatment options for this aggressive disease.
Introduction
Mucosal melanoma is a rare disease, accounting for only 0.03% of new cancer diagnoses, and it is distinct from melanomas that develop at other sites in the body. While melanocytes are most abundant in the skin, they are also present in smaller numbers in the mucous membranes of the respiratory, gastrointestinal, and urogenital tracts, as well as in the eye. Melanocytes in any of these locations have the potential to transform into melanoma. However, it is now clear that melanomas arising from different sites are epidemiologically and genetically distinct. In addition, they differ in how they interact with the immune system and respond to various forms of therapy.
Epidemiology
Of the estimated 87,110 cases of melanoma to be diagnosed in the United States in 2017, less than 2% will arise in the mucosal surfaces of the body.[1-3] While melanomas can develop within any mucosal surface, the vast majority arise in the mucosae of the head and neck (31% to 55%), anorectal (17% to 24%), and vulvovaginal (18% to 40%) regions.[1,2] Less frequent sites of origin include the mucosae of the pharynx, larynx, urinary tract, cervix, esophagus, and gallbladder.
The epidemiology of mucosal melanoma is distinct from that of its cutaneous counterpart, reflecting biological differences between these diseases (Table 1). Mucosal melanoma tends to develop later in life compared with cutaneous melanoma, with a median age at diagnosis of 70 vs 55 years.[1] Whereas the incidence of cutaneous melanoma has increased at a faster rate than that of any other cancer in the United States, the incidence of mucosal melanoma has remained stable.[4] Mucosal melanoma is more often diagnosed at an advanced stage of disease and is associated with worse outcomes.[2] While the 5-year overall survival rate for cutaneous melanoma is 80%, the rate for mucosal melanoma is only 25%.[1] The inferior outcomes may be related to the generally more advanced disease at time of diagnosis, anatomic factors complicating complete resection, the rich lymphovascular supply of the mucosal surfaces, and other biological factors. Interestingly, in addition to having an inferior survival from the time of diagnosis, patients with mucosal melanoma may have a poorer stage-matched survival than other melanoma subtypes from the time of development of clinical metastatic disease.[5]
Whereas cutaneous melanoma is slightly more common in men than women, the incidence rate of mucosal melanoma is 87% higher in women than men. This increased incidence is due to higher rates of genital tract melanomas in women.[2,6,7] There are also significant racial disparities in incidence rates. Mucosal melanomas account for 5% to 13% of melanomas in black patients, 23% of melanomas in Chinese patients, and only 1% to 2% of melanomas in white patients.[2,8] These differences are reflective of the lower incidence rates of cutaneous melanoma in non-white groups. In fact, the absolute incidence rate of mucosal melanoma is twice as high in white compared with black individuals.[2] Unlike cutaneous melanoma, which is more common in southern and coastal states, mucosal melanoma has no consistent predilection for any particular geographic area. One study suggested that the incidence of anorectal melanoma is associated with more northern latitudes; however, a more recent study found the opposite to be the case.[9,10] While cutaneous melanoma is associated with exposure to ultraviolet (UV) radiation, no clear environmental risk factors have been identified for mucosal melanoma[11]; however, having a family history of cutaneous melanoma may increase one’s risk of developing vulvovaginal and anorectal mucosal melanoma.[12]
Anatomy of the Mucosal Immune System
The mucosal immune system is unique, complex, and distinct from that of the skin, and one could hypothesize that features of this distinctive immune system may affect the biology of melanoma arising in mucosal surfaces. When considering the anatomy of the mucosal immune system, sites can be defined as either inductive or effector sites. Inductive sites include regions such as mucosa-associated lymphoid tissue (MALT) and local/regional mucosa-draining lymph nodes, where antigens from mucosal surfaces stimulate naive T and B lymphocytes.[13] Effector sites include areas such as the lamina propria, exocrine gland stroma, and surface epithelia, where mature lymphocytes perform their functions, such as releasing cytokines and secreting antibodies.[13,14]
Throughout the mucosa of the gastrointestinal tract, a very particular balance must be continuously maintained in order to regulate immune reactions to a wide array of both harmless and potentially harmful antigens. This regulation of immune reactions is known as immune tolerance. Despite high bacterial colonization with both commensal and pathologic microbes, as well as frequent contact with antigens from food protein, acute inflammatory and allergic reactions are rarely seen in the mucosa of the gastrointestinal tract.[14] In the gut, the release of cytokines and chemokines is important in initiating an adaptive immune response. When antigens are presented to T lymphocytes by antigen-presenting cells, the presence or absence of inflammation determines whether or not the immune system is activated. During exposure to food antigens or nonpathogenic microbes, inflammation is absent, which results in immune tolerance-the default response.[15] There are three possible mechanisms by which tolerance is effected in both the gut and oral mucosa. These include T-cell depletion by apoptosis; anergy (ie, the process by which T cells that are presented with a peptide in the absence of costimulatory signals become refractory to further stimulation with the antigen and are therefore inactivated); and the development of regulatory T cells, which can actively suppress antigen-specific responses following re-challenge with the antigen.[14,15]
Mucosal Melanoma of the Head and Neck
The head and neck region is the most common site for mucosal melanoma in men and the second most common site in women, although mucosal melanomas represent only 0.5% of all head and neck cancers.[2,16] The incidence of mucosal melanomas of the head and neck is 0.7 to 0.9 cases per million people per year and is not significantly different between men and women.[2] The median age at diagnosis of mucosal melanoma of the head and neck ranges from 60 to 69 years. Interestingly, melanoma of the oral cavity typically presents at a younger age, with as many as 18% of cases occurring in persons aged 40 years or younger.[17,18]
Sinonasal melanomas constitute 70% of mucosal melanomas of the head and neck, with 80% arising in the nasal cavity.[2,16,19] Within the nasal cavity, the turbinates and nasal wall are most commonly involved, followed by the nasal septum. Of the sinuses, the maxillary sinus is most often involved, followed by the ethmoid, frontal, and sphenoid sinuses. Oral cavity melanomas make up almost 30% of mucosal melanomas of the head and neck, and usually involve the palate and maxillary gingiva.[2,17,19] Preexisting melanosis is seen in about one-third of patients with oral melanoma.[17] While use of alcohol and tobacco have been shown to increase one’s risk of developing squamous cell carcinoma of the head and neck, no similar evidence exists for mucosal melanoma.[17,20] The 5-year overall survival rate for mucosal melanoma of the head and neck ranges from 17% to 35%. The prognosis, however, appears to vary by site, with nasal cavity disease having a relatively better prognosis and sinus disease having an inferior prognosis.[19,21,22]
Anatomically, the mucosa of the head and neck can be divided into a layer of stratified squamous epithelium and an underlying connective tissue layer known as the lamina propria (Table 2). The oral mucosa does not contain MALT. Instead, immune responses are induced in the local and regional lymph nodes (ie, the tonsils, adenoids, and cervical lymph nodes). The majority of Langerhans cells can be found in the mucosal surfaces lining the oral cavity.[13,23] Studies show higher Toll-like receptor (TLR)2 and TLR4 expression on oral Langerhans cells compared with Langerhans cells of the epidermis in steady state. When TLRs are triggered by lipopolysaccharides, oral Langerhans cells upregulate expression of coinhibitory molecules B7-H1 and B7-H3, whereas expression of the costimulatory molecule CD86 (B7-2) is decreased. This leads to regulatory T-cell development, subsequent interleukin (IL)-10 and transforming growth factor beta secretion, and ultimate suppression of the immune response.[23]
Vulvovaginal Mucosal Melanoma
The incidence of genitourinary melanomas is approximately 10 times higher in women (2 cases/1 million person-years) than in men (0.2 cases/1 million person-years).[2,24,25] Genitourinary melanomas account for 57% of mucosal melanomas and 1.3% to 7% of all melanomas in women.[2,26] Of these cases, 77% arise in the vulva and 5% to 20% arise in the vagina, with a smaller number arising elsewhere-primarily in the cervix.[2,27] The median age at diagnosis of vulvovaginal mucosal melanoma is 66 years, with vaginal melanomas most often developing in the sixth and seventh decades and vulvar melanomas in the seventh decade.[25,28,29] The 5-year overall survival rate for vulvovaginal melanoma is 36%, with better outcomes for vulvar melanoma than vaginal melanoma.[4,24,26]
After squamous cell carcinoma, melanoma is the second most common cancer of the vulva, accounting for 3.4% to 10% of vulvar malignancies.[29] Eighty-five percent of vulvar melanomas arise in the labia minora; the clitoris; or the inner, glabrous, nonhairy portion of the labia majora; the remaining 15% arise in the outer, nonglabrous, hair-bearing portion of the labia majora.[26] Vaginal melanomas, with an estimated incidence rate of 0.26 cases per million women per year, account for less than 3% of vaginal tumors and comprise up to 1% of all melanomas in women. Vaginal melanomas most commonly arise in the lower third of the vagina on the anterior wall.[28]
The mucosal lining of the female genital tract differs from that of the gastrointestinal tract in terms of cellular composition, microflora, and effector mechanisms of innate and adaptive immunity, although it should be noted that the immunologic anatomy and biology of the genital, anal, and lower rectal tract mucosae are less well defined than those of the remainder of the gastrointestinal tract.[30] In general, the mucosal surfaces of the female genital tract can be divided into two distinct types, and the dividing line between the two occurs at the transformation zone.[31] Type I mucosal surfaces line the uterus, endocervix, and upper rectum, and consist of a single layer of tightly joined, simple columnar epithelium. In contrast, type II mucosal surfaces line the outer vagina, inner vagina, and ectocervix, and consist of multiple layers of stratified squamous epithelium.[31,32] The additional layers protect against tissue abrasion, and the lack of tight junctions allows for the free movement of molecules between cells.[32]
Unlike type I mucosal surfaces, type II mucosae lack MALT and immunoglobulin (Ig)A transport systems. Because of the absence of MALT in type II mucosal tissue, initiation of an adaptive immune response occurs in the draining lymph nodes. These include the common iliac, interiliac, external iliac, and inguinal femoral lymph nodes in the vaginal canal.[31] Due to the lack of IgA transporter systems in type II epithelium, IgA is secreted from adjacent type I epithelium. In addition, serum-derived IgG, which is produced locally, diffuses paracellularly through type II mucosal tissue in the female genital tract in particular.[31] Recent studies show that the vaginal mucosa can support T-cell induction in the absence of MALT or secondary lymphoid tissues, suggesting that the type II vaginal mucosa can itself act as an inductive site for the generation of primary CD8+ T-cell immune responses. Whether these induced CD8+ T cells originate from local naive T cells or migrate from other nonlymphoid tissue compartments remains unknown. Still, these studies suggest that it may be possible to induce local immunity without systemic immune activation.[30]
Anorectal Mucosal Melanoma
Anorectal melanomas account for 0.2% to 1.3% of all melanomas and 1% of all anorectal cancers.[1,2,33] Between 39% and 42% of anorectal melanomas are located within the rectum, one-third arise in the anal canal, and the remainder have an indeterminate site of origin.[9,34] The incidence of anorectal melanoma increases with age, and the average age at diagnosis is 68 to 72 years.[33,34] Unlike other mucosal melanomas, anorectal melanomas have been increasing in frequency in recent decades.[34,35] Women are 1.6 to 2.3 times more likely to develop anorectal melanoma than men. Hispanic whites are at greatest risk; African Americans and non-Hispanic whites fall in the middle.[2,9,34] HIV infection may be a risk factor.[33] Anorectal melanomas tend to have a poor prognosis, with a 5-year overall survival rate of approximately 20%.[36,37]
As with the mucosae of the vulvovaginal region, type I and type II nomenclature is also used to describe the mucosae of the anorectal canal. The anorectal mucosal surfaces are similar in terms of cellular composition and immune function to those of the vaginal canal. Type I mucosal surfaces line the upper rectum and consist of a single layer of tightly joined, simple columnar epithelium, while type II mucosal surfaces line the lower rectum and anus and consist of multiple layers of stratified squamous epithelium.[31,32] The dividing line between the two tissue types occurs at the anorectal junction. Unlike the type I cervix, whose mucus comes from glands in its crypts, type I rectum is lubricated by goblet cells. Furthermore, type II anorectal surfaces are drained by the inguinal lymph nodes because of their lack of MALT.[30]
Molecular Biology of Mucosal Melanoma
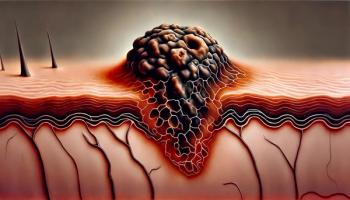
A distinct pattern of genetic abnormalities mirrors the distinct epidemiologic and clinical features of mucosal melanoma. One of the most striking genetic features of mucosal melanoma is its relatively low mutational burden when compared with cutaneous disease. With an average 86,495 single-nucleotide variants (SNVs) per tumor, cutaneous melanoma has one of the highest somatic mutation rates of any cancer. Mucosal melanoma, by contrast, has an average of 8,193 SNVs per tumor, more than 10-fold fewer mutations.[38-40] This discrepancy most likely reflects the fact that different factors lead to oncogenesis in the two types of melanoma. Cancers related to chronic mutagenic exposures, such as lung cancer (tobacco smoke) and cutaneous melanoma (UV radiation), have the highest rates of somatic mutations.[39] The lower mutational burden of mucosal melanoma is similar to that observed in breast and prostate cancers, which are not associated with known environmental carcinogens. Furthermore, the majority of mutations in cutaneous melanoma are C → T transitions at pyrimidine dimers, a pattern characteristic of UV-induced DNA damage; mucosal melanoma is not enriched in this mutational pattern.
Another distinctive genetic feature of mucosal melanoma is its high rate of copy number and structural variants, demonstrated both by array-based comparative genomic hybridization and whole-genome sequencing.[38,41] While gene amplifications are rare in cutaneous melanoma, they are present in approximately 85% of mucosal melanomas.[41] Along the same lines, mucosal melanoma has an average of 3.7 times as many structural variants as its cutaneous counterpart.[38] The cause of this increased chromosomal instability has yet to be elucidated.
While mutational burden has important implications for treatment with immunotherapy, the presence of specific driver mutations is also of major therapeutic relevance (Table 3). BRAF is a targetable oncogene in the RAF/MEK/ERK pathway.[41] Approximately 50% of cutaneous melanomas have an activating BRAF mutation, with an additional 10% to 20% having an activating mutation in NRAS; NRAS is an upstream partner of BRAF that also activates the phosphatidylinositol 3-kinase (PI3K)/Akt/mammalian target of rapamycin (mTOR) pathway.[42] In contrast, only 3% to 11% of mucosal melanomas have BRAF mutations, with another 5% to 14% having NRAS mutations.[41,43,44] Conversely, amplifications and activating mutations of KIT are observed in 14% to 39% of mucosal melanomas and are only rarely observed in melanomas arising in skin that receives intermittent sun exposure.[42-46] KIT, a type III transmembrane receptor tyrosine kinase that sits upstream of NRAS and BRAF, feeds into several signaling pathways, including both the RAS/RAF/MEK/ERK cascade and the PI3K/Akt/mTOR pathway.[41,47] A recent study found that 20% of anorectal melanomas have inactivating mutations in NF1, a tumor suppressor gene that negatively regulates the RAS/RAF/MEK/ERK pathway activity.[45] Mutations in BRAF, RAS, KIT, and NF1 are almost always mutually exclusive, suggesting that each of them is of functional significance.[42,45]
A recent study reported that 9.5% of mucosal melanomas arising in a Chinese patient population had mutations in either GNAQ or GNA11, and that these mutations were associated with poor prognosis.[48] Mutations in GNAQ or GNA11 occur in the majority of uveal melanomas and drive oncogenesis via activation of the phospholipase C/protein kinase C (PKC), Rho/Rac, and Yes-associated protein pathways.[49] Mutations in SF3B1, also previously identified in uveal melanoma, have been reported to be present in approximately 20% of anorectal melanomas.[45] SF3B1 encodes subunit 1 of the RNA splicing factor 3b protein complex, but the functional consequences of its mutation remain to be fully elucidated.
CCND1, which encodes cyclin D1, is amplified in a number of melanomas with wild-type BRAF and NRAS. Similarly, CDK4, which encodes cyclin-dependent kinase 4, a targetable binding partner of cyclin D1, is more commonly amplified in mucosal than in cutaneous melanomas. CDK4 amplification is seen neither in conjunction with mutations in NRAS or BRAF, nor with CCND1 amplification, implying that only one of these genetic abnormalities is necessary for malignant progression.[41]
Management of Primary Disease
Surgery remains the primary therapeutic intervention for mucosal melanoma. As in cutaneous disease, complete resection offers the best chance for prolonged disease-free survival and cure. Unfortunately, wide negative margins are often difficult to achieve in mucosal melanoma due to anatomic constraints, disease multifocality, and/or a lentiginous growth pattern, and most mucosal melanomas recur regardless of initial locoregional management.[50,51]
Radiotherapy may play a role in the definitive treatment of unresectable, locally advanced mucosal melanoma; it can also be used as adjuvant treatment after surgical resection. Definitive radiation is associated with complete response in approximately 30% of cases of mucosal melanoma arising from the head and neck, with local control achieved in 40% of cases.[52,53] Conventionally fractionated radiation is commonly given for unresectable mucosal melanoma, particularly for sinonasal disease that is in close approximation to the optic apparatus-out of concern for radiation-induced visual complications-with high-risk areas treated to 66 Gy at 2.2 Gy per fraction or 70 Gy at 2 Gy per fraction, and low-risk areas treated to 44–50 Gy at 2 Gy per fraction or 54–63 Gy at 1.6–1.8 Gy per fraction.[54] Alternate radiation fractionation schedules may be considered for mucosal melanoma because of the relative radioresistance of this disease. The Northern Japan Radiation Therapy Oncology Group reported that doses of 3 Gy or more per fraction were more effective at achieving local control than conventionally fractionated radiation, and that survival may be improved with such doses in younger patients.[52] Given the proximity of uninvolved critical organs, advanced treatment modalities such as intensity-modulated radiation or proton therapy may be considered. A pilot study of definitive proton therapy (60 GyE in 15 fractions) for mucosal melanoma of the head and neck demonstrated a 3-year survival rate of 58% and local treatment failure in only 1 of 14 patients, without unacceptable treatment toxicity.[55]
Adjuvant Therapy Considerations
The role of adjuvant systemic therapy in patients with mucosal melanoma following definitive therapy is not clear. The only randomized study of adjuvant chemotherapy in mucosal melanoma demonstrated significantly increased relapse-free and overall survival in patients receiving temozolomide and cisplatin, as compared with interferon alfa-2b or observation. Median relapse-free survival in the chemotherapy group was 20.8 months vs 9.4 months and 5.4 months in the interferon and observation groups, respectively.[56] However, these findings have not been reproduced to date and it is not known whether the impressive results from this single-center Chinese trial are generalizable to other populations. Although lack of effectiveness in the advanced setting does not preclude efficacy in the adjuvant setting, our retrospective single-center study of advanced mucosal melanoma yielded an objective response rate of only 10% to alkylator-based cytotoxic therapy, suggesting a general lack of efficacy for chemotherapy in this disease.[5]
Adjuvant radiation after local excision for mucosal melanoma can be considered, particularly in cases in which surgical margins may be inadequate due to anatomical constraints, as is common in melanomas that arise in the mucosa of the head and neck. For melanomas that arise in the sinonasal mucosa, Moreno et al found that conventionally fractionated radiation to a dose of at least 54 Gy achieved superior locoregional control (45.4%) compared with hypofractionated radiation (0%).[57] The postoperative use of radiotherapy for anorectal melanoma following wide local excision has been reported to be associated with high rates of locoregional control (74% to 82%) at 5 years, with nearly all patients avoiding the need for abdominoperineal resection and permanent colostomy.[58,59] In this setting, treatment to the primary site and pelvic lymph nodes is recommended, with a suggested radiation dose of 25–30 Gy in 5 or 6 fractions (5–6 Gy per fraction). Extending the radiation fields to the inguinal nodes, as is typical for squamous cell carcinoma of the anus, did not demonstrate any improvement in disease outcome but was associated with increased lymphedema and is therefore not routinely done.[58] There are few data regarding the use of radiotherapy for vulvovaginal mucosal melanoma; however, the Gynecologic Cancer InterGroup consensus recommended consideration of neoadjuvant hypofractionated radiation in order to achieve a less radical local excision.[60]
Systemic Therapy for Advanced Disease
Treatment options for advanced mucosal melanoma historically have been extremely limited. Studies of standard chemotherapy regimens such as dacarbazine and paclitaxel/carboplatin showed response rates for mucosal melanomas that were comparable to those seen in cutaneous melanomas.[61,62] Small retrospective studies of biochemotherapy (cisplatin, vinblastine, dacarbazine, interferon alfa-2b, and IL-2) also demonstrated activity that was similar in cutaneous and mucosal melanomas.[63-65] Recent advances in immunotherapy and the identification of actionable genetic alterations have, however, yielded new, more promising therapeutic approaches (Table 4).
Targeted treatment strategies
Our group treated 11 patients with advanced mucosal melanoma harboring KIT alterations as part of our completed phase II trial of imatinib. Of these patients, 1 achieved a durable complete response (95 weeks), 1 achieved a durable partial response (53 weeks), 1 had a transient partial response, and 3 had stable disease at the conclusion of the trial.[44] Two other phase II clinical trials evaluated the efficacy of imatinib in patients with melanoma-including mucosal melanomas-harboring KIT mutations and/or amplifications, with a subset of cases involving mucosal primaries, and both found a disease control rate of approximately 50%.[66,67] Although responses were highly variable, patients with mutations more frequently achieved a clinical response than did those with amplifications, and patients with tumor mutations affecting exons 11 and 13 were able to achieve significant radiographic responses in over 40% of cases.[68] Other KIT inhibitors, such as sorafenib, dasatinib, and sunitinib, have also been reported to have beneficial effects in mucosal melanomas harboring KIT mutations.[69-71]
Unfortunately, even those who initially respond to KIT inhibition ultimately experience disease progression. Mechanisms of secondary resistance to KIT inhibition have not been extensively studied. Reported mechanisms include acquisition of a secondary NRAS Q61K mutation and upregulation of the mTOR pathway.[69,72] In gastrointestinal stromal tumors (GIST), secondary resistance to KIT inhibition is caused primarily by development of additional KIT mutations. The use of alternative KIT inhibitors following progression on imatinib has achieved clinical benefit in patients with advanced GIST.[73,74] There is some evidence that this strategy may prove useful in mucosal melanoma as well. In one report, a patient with an L576P KIT mutation in whom imatinib therapy had previously failed experienced marked reduction in tumor burden in response to dasatinib treatment.[70] Additionally, our phase II study of nilotinib in melanomas refractory or intolerant to a prior KIT inhibitor found partial responses in 18% of patients and disease control for 4 months in 27%.[75]
Other mutations commonly found in mucosal melanoma have the potential to be targeted by small-molecule inhibitors. As in cutaneous melanoma, mucosal melanomas harboring BRAF V600 mutations may respond well to combined BRAF and MEK inhibition. Importantly, these agents have not been tested specifically in patients with mucosal melanoma, and it is unclear whether biological differences between cutaneous and mucosal melanoma might lead to differing responses to these treatment strategies.
Additional rational strategies could be suggested based upon other underlying molecular changes. Mucosal melanomas harboring NF1 mutations could also be targeted with MEK inhibitors. Mucosal melanomas with mutations in CDK4 may respond to palbociclib or ribociclib, which have demonstrated activity in advanced hormone receptor–positive, human epidermal growth factor receptor 2–negative breast cancer. Finally, PKC or MEK inhibitors may be useful in treating mucosal melanomas with GNAQ/GNA11 mutations.
Immunologic treatment strategies
Immunologic checkpoint blockade with anti–cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4) or anti–programmed death 1 (PD-1)/programmed death ligand 1 (PD-L1) agents seems to have some degree of clinical efficacy in advanced mucosal melanoma, although data are limited to smaller retrospective series or subset analyses of prospective trials. Our multicenter retrospective analysis evaluated 33 patients with advanced mucosal melanoma who received ipilimumab, the majority of whom had been pretreated with at least one prior line of therapy. Of the 30 evaluable patients, 1 patient achieved a complete response, 1 had a partial response, and 6 patients had stable disease by immune-related response criteria.[76] An evaluation of 71 patients with metastatic mucosal melanoma treated with ipilimumab through an expanded access program in Italy reported a response rate of 12% and a disease control rate of 36% at a median follow-up time of 21.8 months. The median progression-free survival was 4.3 months, and median overall survival was 6.4 months.[77]
The anti–PD-1/PD-L1 agents have also demonstrated clinical efficacy in advanced mucosal melanoma. A recent retrospective multicenter study evaluated the efficacy of anti–PD-1 agents in rare subtypes of melanoma, including 35 patients with mucosal melanoma and 25 patients with acral melanoma.[78] Of the mucosal melanoma patients, the majority (69%) had M1c disease and had wild-type BRAF, NRAS, and KIT (74%). Within the mucosal melanoma subgroup, there were 8 partial responses (23%) and 7 patients with stable disease (20%), but no complete responses were observed. The median progression-free survival was 3.9 months, and median overall survival was 12.4 months.[78] Therapy was well tolerated, with only 2 patients requiring discontinuation of therapy because of toxicity. Although these studies were limited to small patient numbers, given the rarity of this disease, PD-1 pathway blockade seems to have clinical efficacy in mucosal melanoma, with a tolerable safety profile.
KEY POINTS
- Mucosal melanoma is an aggressive disease that is associated with worse outcomes compared with cutaneous melanoma. The inferior outcomes may be related to diagnosis at a more advanced disease stage, anatomic factors complicating complete resection, the rich lymphovascular supply of the mucosal surfaces, and the unique driver mutations prevalent in this cancer subtype.
- One of the most striking genetic features of mucosal melanoma is its relatively low mutational burden compared with cutaneous disease. Another distinctive feature is its high rate of copy number and structural variants.
- Effective locoregional control can be obtained through complete surgical resection. However, radiotherapy may be appropriate in the adjuvant setting, as wide negative margins may be difficult to achieve. In advanced mucosal melanoma, combination anti–PD-1 and anti–CTLA-4 treatment may be the preferred approach in those who are able to tolerate more aggressive therapies, given the higher response rates observed compared with single-agent checkpoint blockade. The potential for synergy between immunologic checkpoint blockade and radiotherapy is also being explored.
In the largest analysis of PD-1 blockade in mucosal melanoma to date, patients treated in clinical studies with either nivolumab monotherapy or nivolumab combined with ipilimumab were evaluated in a pooled analysis.[79] A total of 86 patients with advanced mucosal melanoma were included in the nivolumab monotherapy analysis, and 35 patients with mucosal melanoma were included in the combination therapy analysis; in addition, outcomes in these patients were compared with outcomes in patients with cutaneous melanoma who were treated in these clinical studies. With nivolumab monotherapy, the observed objective response rate was 23.3% in the mucosal melanoma group compared with 40.9% in the cutaneous melanoma group. The median progression-free survival was 3.0 months and 6.2 months for the mucosal and cutaneous melanoma groups, respectively. Response rates with combined nivolumab and ipilimumab were higher than with nivolumab monotherapy in both melanoma subtypes. The objective response rate was 37.1% and 60.4% in the mucosal and cutaneous melanoma groups, respectively, and median progression-free survival was 5.9 months vs 11.7 months.[79] Interestingly, PD-L1 expression differed between the mucosal and cutaneous melanoma groups, with fewer mucosal melanoma patients being PD-L1–positive (17.4% and 28.6% with ≥ 5% PD-L1 expression in the nivolumab monotherapy group and combination group, respectively) compared with the cutaneous melanoma population (34.3% and 36.8% with ≥ 5% PD-L1 expression in the nivolumab monotherapy and combination groups, respectively). In general, the response rates were higher in the ≥ 5% PD-L1 mucosal melanoma group, although responses were still observed in the < 5% PD-L1 group among both patients who received monotherapy and those who received combination therapy. Much as in cutaneous melanoma, the role of PD-L1 status as an immune biomarker in mucosal melanoma remains unclear.[79]
The potential for synergy with the combination of immunologic checkpoint blockade and radiotherapy has gained significant attention. Our case series of combined immunotherapy and radiation for mucosal melanoma of the lower genital tract, which demonstrated complete radiographic response in all patients treated, and a complete pathologic response in one patient at the time of surgery, suggests that further studies should be pursued in this area.[80]
Conclusion
Mucosal melanoma is a unique disease that requires clinical considerations distinct from other melanoma subtypes. Its characteristically low mutational burden, high copy number and structural variants, and unique driver mutation prevalence are important in helping us understand the natural history of the disease and its response to various therapies. Other critical factors to consider include the mucosal immune system and the potential impact of a tolerogenic microenvironment on the development and progression of disease.
Effective locoregional control can be obtained through complete surgical resection, although wide negative margins may be difficult to achieve. Therefore, radiotherapy may be appropriate in the adjuvant setting; in cases where lesions are unresectable, definitive radiotherapy should be considered. Despite aggressive locoregional management, recurrent disease is common and treatment in this setting remains challenging. Routine molecular profiling for BRAF and KIT is recommended and may identify potential targeted therapy options. Immunologic checkpoint blockade has demonstrated clinical efficacy in advanced mucosal melanoma, although activity appears to be lower compared with what has been observed in cutaneous melanoma. Combination anti–PD-1 and anti–CTLA-4 treatment may be the preferred approach in those who are able to tolerate more aggressive therapies, given the higher response rates observed compared with single-agent checkpoint blockade.
Overall, despite the dramatic therapeutic advances made elsewhere in the melanoma field, the poor prognosis of patients with mucosal melanoma mandates continued emphasis on laboratory and clinical research efforts in this rare subset of disease.
Financial Disclosure: Dr. Carvajal serves as a consultant to AstraZeneca, Bristol-Myers Squibb, Iconic Therapeutics, Janssen Novartis, Merck, and Roche/Genentech; and as an advisory board member for Aura Bioscience, Chimeron, and Rgenix. The other authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
1. Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer. 1998;83:1664-78.
2. McLaughlin CC, Wu XC, Jemal A, et al. Incidence of noncutaneous melanomas in the U.S. Cancer. 2005;103:1000-7.
3. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin. 2017;67:7-30.
4. Patrick RJ, Fenske NA, Messina JL. Primary mucosal melanoma. J Am Acad Dermatol. 2007;56:828-34.
5. Shoushtari AN, Bluth MJ, Goldman DA, et al. Clinical features and response to systemic therapy in a historical cohort of advanced or unresectable mucosal melanoma. Melanoma Res. 2017;27:57-64.
6. Pandey M, Mathew A, Abraham EK, et al. Primary malignant melanoma of the mucous membranes. Eur J Surg Oncol. 1998;24:303-7.
7. Sutherland CM, Chmiel JS, Henson DE, Winchester DP. Patient characteristics, methods of diagnosis, and treatment of mucous membrane melanoma in the United States of America. J Am Coll Surg. 1994;179:561-6.
8. Chi Z, Li S, Sheng X, et al. Clinical presentation, histology, and prognoses of malignant melanoma in ethnic Chinese: a study of 522 consecutive cases. BMC Cancer. 2011;11:85.
9. Callahan A, Anderson WF, Patel S, et al. Epidemiology of anorectal melanoma in the United States: 1992 to 2011. Dermatol Surg. 2016;42:94-9.
10. Weinstock MA. Epidemiology and prognosis of anorectal melanoma. Gastroenterology. 1993;104:174-8.
11. Garland CF, Garland FC, Gorham ED. Epidemiologic evidence for different roles of ultraviolet A and B radiation in melanoma mortality rates. Ann Epidemiol. 2003;13:395-404.
12. Cazenave H, Maubec E, Mohamdi H, et al. Genital and anorectal mucosal melanoma is associated with cutaneous melanoma in patients and in families. Br J Dermatol. 2013;169:594-9.
13. Brandtzaeg P, Kiyono H, Pabst R, Russell MW. Terminology: nomenclature of mucosa-associated lymphoid tissue. Mucosal Immunol. 2008;1:31-7.
14. Novak N, Haberstok J, Bieber T, Allam JP. The immune privilege of the oral mucosa. Trends Mol Med. 2008;14:191-8.
15. Janeway CA Jr, Travers P, Walport M, et al. The mucosal immune system. In: Immunobiology: the Immune System in Health and Disease. New York: Garland Science; 2001.
16. Plavc G, But-Hadžic J, Anicin A, et al. Mucosal melanoma of the head and neck: a population-based study from Slovenia, 1985-2013. Radiat Oncol. 2016;11:137.
17. Rapini RP, Golitz LE, Greer RO, et al. Primary malignant melanoma of the oral cavity: a review of 177 cases. Cancer. 1985;55:1543-51.
18. Gilligan D, Slevin NJ. Radical radiotherapy for 28 cases of mucosal melanoma in the nasal cavity and sinuses. Br J Radiol. 1991;64:1147-50.
19. Patel SG, Prasad ML, Escrig M, et al. Primary mucosal malignant melanoma of the head and neck. Head Neck. 2002;24:247-57.
20. Hashibe M, Brennan P, Chuang SC, et al. Interaction between tobacco and alcohol use and the risk of head and neck cancer: pooled analysis in the International Head and Neck Cancer Epidemiology Consortium. Cancer Epidemiol Biomarkers Prev. 2009;18:541-50.
21. Wu AJ, Gomez J, Zhung JE, et al. Radiotherapy after surgical resection for head and neck mucosal melanoma. Am J Clin Oncol. 2010;33:281-5.
22. Benlyazid A, Thariat J, Temam S, et al. Postoperative radiotherapy in head and neck mucosal melanoma: a GETTEC study. Arch Otolaryngol Head Neck Surg. 2010;136:1219-25.
23. Hovav AH. Dendritic cells of the oral mucosa. Mucosal Immunol. 2014;7:27-37.
24. Vyas R, Thompson CL, Zargar H, et al. Epidemiology of genitourinary melanoma in the United States: 1992 through 2012. J Am Acad Dermatol. 2016;75:144-50.
25. Sanchez A, RodrÃguez D, Allard CB, et al. Primary genitourinary melanoma: epidemiology and disease-specific survival in a large population-based cohort. Urol Oncol. 2016;34:166.e7-e14.
26. Ragnarsson-Olding BK, Kanter-Lewensohn LR, Lagerlöf B, et al. Malignant melanoma of the vulva in a nationwide, 25-year study of 219 Swedish females: clinical observations and histopathologic features. Cancer. 1999;86:1273-84.
27. Weinstock MA. Malignant melanoma of the vulva and vagina in the United States: patterns of incidence and population-based estimates of survival. Am J Obstet Gynecol. 1994;171:1225-30.
28. Piura B, Rabinovich A, Yanai-Inbar I. Primary malignant melanoma of the vagina: case report and review of literature. Eur J Gynaecol Oncol. 2002;23:195-8.
29. Sugiyama VE, Chan JK, Shin JY, et al. Vulvar melanoma: a multivariable analysis of 644 patients. Obstet Gynecol. 2007;110:296-301.
30. Wang Y, Sui Y, Kato S, et al. Vaginal type-II mucosa is an inductive site for primary CD8+ T-cell mucosal immunity. Nat Commun. 2015;6:6100.
31. Iwasaki A. Antiviral immune responses in the genital tract: clues for vaccines. Nat Rev Immunol. 2010;10:699-711.
32. Deruaz M, Luster AD. Chemokine-mediated immune responses in the female genital tract mucosa. Immunol Cell Biol. 2015;93:347-54.
33. Cagir B, Whiteford MH, Topham A, et al. Changing epidemiology of anorectal melanoma. Dis Colon Rectum. 1999;42:1203-8.
34. Coté TR, Sobin LH. Primary melanomas of the esophagus and anorectum: epidemiologic comparison with melanoma of the skin. Melanoma Res. 2009;19:58-60.
35. Chen H, Cai Y, Liu Y, et al. Incidence, surgical treatment, and prognosis of anorectal melanoma from 1973 to 2011: a population-based SEER analysis. Medicine (Baltimore). 2016;95:e2770.
36. Zhang S, Gao F, Wan D. Effect of misdiagnosis on the prognosis of anorectal malignant melanoma. J Cancer Res Clin Oncol. 2010;136:1401-5.
37. Row D, Weiser MR. Anorectal melanoma. Clin Colon Rectal Surg. 2009;22:120-6.
38. Furney SJ, Turajlic S, Stamp G, et al. Genome sequencing of mucosal melanomas reveals that they are driven by distinct mechanisms from cutaneous melanoma. J Pathol. 2013;230:261-9.
39. Alexandrov LB, Nik-Zainal S, Wedge DC, et al. Signatures of mutational processes in human cancer. Nature. 2013;500:415-21.
40. Krauthammer M, Kong Y, Ha BH, et al. Exome sequencing identifies recurrent somatic RAC1 mutations in melanoma. Nat Genet. 2012;44:1006-14.
41. Curtin JA, Fridlyand J, Kageshita T, et al. Distinct sets of genetic alterations in melanoma. N Engl J Med. 2005;353:2135-47.
42. Curtin JA, Busam K, Pinkel D, Bastian BC. Somatic activation of KIT in distinct subtypes of melanoma. J Clin Oncol. 2006;24:4340-6.
43. Tacastacas JD, Bray J, Cohen YK, et al. Update on primary mucosal melanoma. J Am Acad Dermatol. 2014;71:366-75.
44. Carvajal RD, Antonescu CR, Wolchok JD, et al. KIT as a therapeutic target in metastatic melanoma. JAMA. 2011;305:2327-34.
45. Yang HM, Hsiao SJ, Schaeffer DF, et al. Identification of recurrent mutational events in anorectal melanoma. Mod Pathol. 2017;30:286-96.
46. Santi R, Simi L, Fucci R, et al. KIT genetic alterations in anorectal melanomas. J Clin Pathol. 2015;68:130-4.
47. Flaherty KT, Robert C, Hersey P, et al. Improved survival with MEK inhibition in BRAF-mutated melanoma. N Engl J Med. 2012;367:107-14.
48. Sheng X, Kong Y, Li Y, et al. GNAQ and GNA11 mutations occur in 9.5% of mucosal melanoma and are associated with poor prognosis. Eur J Cancer. 2016;65:156-63.
49. Yoo JH, Shi DS, Grossmann AH, et al. ARF6 is an actionable node that orchestrates oncogenic GNAQ signaling in uveal melanoma. Cancer Cell. 2016;29:889-904.
50. Carvajal RD, Spencer SA, Lydiatt W. Mucosal melanoma: a clinically and biologically unique disease entity. J Natl Compr Canc Netw. 2012;10:345-56.
51. Lee SP, Shimizu KT, Tran LM, et al. Mucosal melanoma of the head and neck: the impact of local control on survival. Laryngoscope. 1994;104:121-6.
52. Wada H, Nemoto K, Ogawa Y, et al. A multi-institutional retrospective analysis of external radiotherapy for mucosal melanoma of the head and neck in Northern Japan. Int J Radiat Oncol Biol Phys. 2004;59:495-500.
53. Christopherson K, Malyapa RS, Werning JW, et al. Radiation therapy for mucosal melanoma of the head and neck. Am J Clin Oncol. 2015;38:87-9.
54. National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines). Head and neck cancers. Version 2.2017. https://www.nccn.org/professionals/physician_gls/pdf/head-and-neck.pdf. Accessed October 5, 2017.
55. Zenda S, Kawashima M, Nishio T, et al. Proton beam therapy as a nonsurgical approach to mucosal melanoma of the head and neck: a pilot study. Int J Radiat Oncol Biol Phys. 2011;81:135-9.
56. Lian B, Si L, Cui C, et al. Phase II randomized trial comparing high-dose IFN-α2b with temozolomide plus cisplatin as systemic adjuvant therapy for resected mucosal melanoma. Clin Cancer Res. 2013;19:4488-98.
57. Moreno MA, Roberts DB, Kupferman ME, et al. Mucosal melanoma of the nose and paranasal sinuses, a contemporary experience from the M. D. Anderson Cancer Center. Cancer. 2010;116:2215-23.
58. Kelly P, Zagars GK, Cormier JN, et al. Sphincter-sparing local excision and hypofractionated radiation therapy for anorectal melanoma: a 20-year experience. Cancer. 2011;117:4747-55.
59. Ballo MT, Gershenwald JE, Zagars GK, et al. Sphincter-sparing local excision and adjuvant radiation for anal-rectal melanoma. J Clin Oncol. 2002;20:4555-8.
60. Leitao MM, Cheng X, Hamilton AL, et al. Gynecologic Cancer InterGroup (GCIG) consensus review for vulvovaginal melanomas. Int J Gynecol Cancer. 2014;24:S117-S122.
61. Chang W, Lee SJ, Park S, et al. Effect of paclitaxel/carboplatin salvage chemotherapy in noncutaneous versus cutaneous metastatic melanoma. Melanoma Res. 2013;23:147-51.
62. Yi JH, Yi SY, Lee HR, et al. Dacarbazine-based chemotherapy as first-line treatment in noncutaneous metastatic melanoma: multicenter, retrospective analysis in Asia. Melanoma Res. 2011;21:223-7.
63. Bartell HL, Bedikian AY, Papadopoulos NE, et al. Biochemotherapy in patients with advanced head and neck mucosal melanoma. Head Neck. 2008;30:1592-8.
64. Kim KB, Sanguino AM, Hodges C, et al. Biochemotherapy in patients with metastatic anorectal mucosal melanoma. Cancer. 2004;100:1478-83.
65. Harting MS, Kim KB. Biochemotherapy in patients with advanced vulvovaginal mucosal melanoma. Melanoma Res. 2004;14:517-20.
66. Hodi FS, Corless CL, Giobbie-Hurder A, et al. Imatinib for melanomas harboring mutationally activated or amplified KIT arising on mucosal, acral, and chronically sun-damaged skin. J Clin Oncol. 2013;31:3182-90.
67. Guo J, Si L, Kong Y, et al. Phase II, open-label, single-arm trial of imatinib mesylate in patients with metastatic melanoma harboring c-Kit mutation or amplification. J Clin Oncol. 2011;29:2904-9.
68. Carvajal RD, Hamid O, Antonescu CR. Selecting patients for KIT inhibition in melanoma. Methods Mol Biol. 2014;1102:137-62.
69. Minor DR, Kashani-Sabet M, Garrido M, et al. Sunitinib therapy for melanoma patients with KIT mutations. Clin Cancer Res. 2012;18:1457-63.
70. Woodman SE, Trent JC, Stemke-Hale K, et al. Activity of dasatinib against L576P KIT mutant melanoma: molecular, cellular, and clinical correlates. Mol Cancer Ther. 2009;8:2079-85.
71. Quintás-Cardama A, Lazar AJ, Woodman SE, et al. Complete response of stage IV anal mucosal melanoma expressing KIT Val560Asp to the multikinase inhibitor sorafenib. Nat Clin Pract Oncol. 2008;5:737-40.
72. Si L, Xu X, Kong Y, et al. Major response to everolimus in melanoma with acquired imatinib resistance. J Clin Oncol. 2012;30:e37-e40.
73. Demetri GD, Reichardt P, Kang YK, et al. Efficacy and safety of regorafenib for advanced gastrointestinal stromal tumours after failure of imatinib and sunitinib (GRID): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:295-302.
74. Demetri GD, van Oosterom AT, Garrett CR, et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet. 2006;368:1329-38.
75. Carvajal RD, Lawrence DP, Weber JS, et al. Phase II study of nilotinib in melanoma harboring KIT alterations following progression to prior KIT inhibition. Clin Cancer Res. 2015;21:2289-96.
76. Postow MA, Luke JJ, Bluth MJ, et al. Ipilimumab for patients with advanced mucosal melanoma. Oncologist. 2013;18:726-32.
77. Del Vecchio M, Di Guardo L, Ascierto PA, et al. Efficacy and safety of ipilimumab 3mg/kg in patients with pretreated, metastatic, mucosal melanoma. Eur J Cancer. 2014;50:121-7.
78. Shoushtari AN, Munhoz RR, Kuk D, et al. The efficacy of anti-PD-1 agents in acral and mucosal melanoma. Cancer. 2016;122:3354-62.
79. D’Angelo SP, Larkin J, Sosman JA, et al. Efficacy and safety of nivolumab alone or in combination with ipilimumab in patients with mucosal melanoma: a pooled analysis. J Clin Oncol. 2017;35:226-35.
80. Schiavone MB, Broach V, Shoushtari AN, et al. Combined immunotherapy and radiation for treatment of mucosal melanomas of the lower genital tract. Gynecol Oncol Rep. 2016;16:42-6.
81. Cancer Genome Atlas Network. Genomic classification of cutaneous melanoma. Cell. 2015;161:1681-96.
82. Jiang D, Ge J, Liao Q, et al. IgG and IgA with potential microbial-binding activity are expressed by normal human skin epidermal cells. Int J Mol Sci. 2015;16:2574-90.
83. Terris B, Potet F. Structure and role of Langerhans cells in the human oesophageal epithelium. Digestion. 1995;56(suppl 1):9-14.