NSCLC Patient Develops Erythema After Vancomycin Infusion
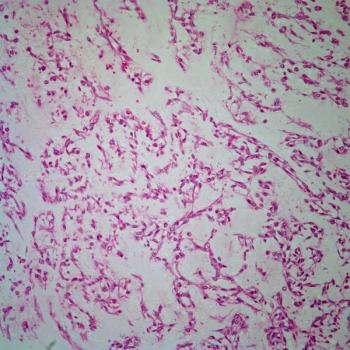
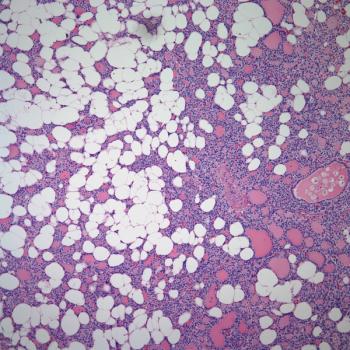
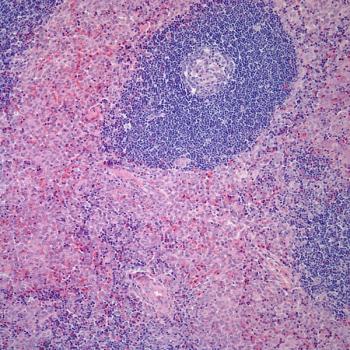
A 71-year-old man with a smoking history of more than 100 pack-years developed non–small-cell carcinoma of the lung, and was 1 month status post lobectomy and undergoing adjuvant double-agent chemotherapy. Comorbidities included obesity and unstable type 2 diabetes mellitus. The patient developed a productive cough, as well as fever (39.4°C [103°F]) and progressive dyspnea, none of which was responsive to outpatient cephalosporin treatment. Pending sputum culture results, intravenous vancomycin was administered in an outpatient infusion center. During his very first infusion (rate of 1 g over 30 minutes) he developed flushing, followed by widespread fixed erythema, muscular spasms in the back, and transient but severe hypotension. The infusion was stopped, and the patient was admitted to the hospital for further evaluation and care. At the time of dermatologic consultation, he had widespread, nontender macular erythema with no scaling, vesiculation, bulla formation, sloughing, or oozing. Mucosae were normal. According to medical history obtained from both the patient and his family, he had never received vancomycin previously. Should he survive this episode, the patient will remain at high risk for further infectious complications, making the question below an important one.
Can he ever receive vancomycin again?
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.