NSCLC Patient Develops Fever and Rash Following Treatment for Brain Metastases
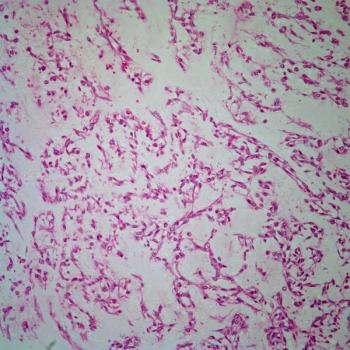
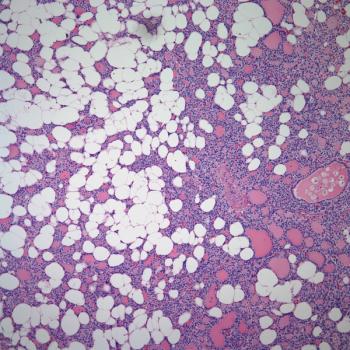
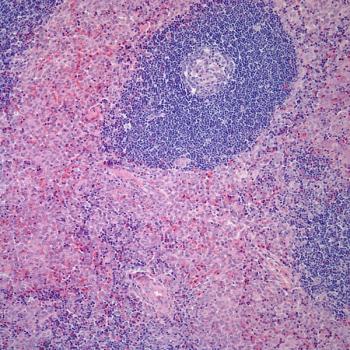
A 40-year-old man had been previously treated at another institution for stage II non-small-cell carcinoma of the lung (adenocarcinoma type) with lobectomy and adjuvant chemotherapy. He was ostensibly disease free for 2 years until he experienced several grand mal (tonic-clonic) seizures. The patient was transported to our institution and hospitalized for evaluation and treatment. Imaging examinations disclosed one large and six small intracerebral metastases. The patient was immediately placed on phenytoin; whole-brain radiotherapy, along with gefitinib (Iressa), was also initiated. Ten days into an anticipated 2-week series of radiotherapy treatments, the patient developed a low-grade fever (100.4°F) and a nonspecific, erythematous, maculopapular eruption involving the radiotherapy port. The rash soon spread to the entire face, chest, upper back, hands, and feet while developing the distinctive morphology shown. The patient also developed purulent conjunctivitis and mildly crusted cheilitis. Neither palpable organomegaly nor facial swelling was present.
This phenomenon most likely represents:
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.