Articles by Scott S. Tykodi, MD, PhD

Panelists discuss how the future of renal cell carcinoma (RCC) treatment lies in developing better biomarkers for patient selection, novel immune therapies including chimeric antigen receptor (CAR) T cells and T-cell engagers, HIF-alpha inhibitors, radioligand therapies, and moving beyond the current immunotherapy-based doublet paradigm that has dominated for 7 years.

Panelists discuss how toxicity considerations significantly influence treatment selection given multiple effective options, requiring personalized discussions about patient goals, comorbidities, and tolerance for different adverse effect profiles between immune therapy doublets and immunotherapy-tyrosine kinase inhibitor (IO-TKI) combinations.

Panelists discuss how favorable-risk patients may be candidates for active surveillance if their disease is indolent, while treatment decisions should consider the long-term survival benefits of ipilimumab plus nivolumab vs the higher response rates of immunotherapy-tyrosine kinase inhibitor (IO-TKI) combinations, with pseudoprogression being relatively rare in clinical practice.

Panelists discuss how treatment selection for a typical intermediate-risk patient with clear cell renal cell carcinoma (RCC) involves choosing between ipilimumab plus nivolumab for long-term durable responses in nonsymptomatic patients and immunotherapy-tyrosine kinase inhibitor (IO-TKI) combinations for those requiring rapid disease control or cytoreduction.

Panelists discuss how the CLEAR trial showed pembrolizumab plus lenvatinib achieved the highest objective response rate (71%) and progression-free survival (23.3 months) among frontline regimens, though requiring careful patient selection due to lenvatinib's challenging toxicity profile at the full 20 mg dose.

Panelists discuss how CheckMate 9ER results demonstrated significant progression-free survival and overall survival benefits with nivolumab plus cabozantinib vs sunitinib, with particularly impressive HRs for patients with visceral disease, including liver, bone, and lung metastases.

Panelists discuss how the KEYNOTE-426 trial established pembrolizumab plus axitinib as an effective and well-tolerated immunotherapy-tyrosine kinase inhibitor (IO-TKI) combination with high response rates and unprecedented tumor control, particularly suitable for frail patients due to axitinib's selective targeting and short half-life.

Panelists discuss how the CheckMate 214 study demonstrated durable overall survival benefits with ipilimumab plus nivolumab vs sunitinib, with 9-year follow-up showing improved outcomes even in favorable-risk patients and nearly half of responders remaining in remission.

Panelists discuss how clear cell renal cell carcinoma (RCC) represents the most common kidney cancer subtype, typically affecting men in their 50s and 60s who often present incidentally with metastatic disease, and has limited identifiable risk factors beyond smoking, hypertension, and obesity.
Drs Thomas Hutson and Scott Tykodi explain when to consider a debulking surgery for patients with renal cell carcinoma.
A look at how to best sequence therapies for renal cell carcinoma from the front-line setting on.
Dr Scott Tykodi provides advice for community oncologists managing patients with renal cell carcinoma.
Thomas Hutson, DO, PharmD, and Scott Tykodi, MD, PhD, discuss their takeaways from the CLEAR trial and how risk category stratification affected the study.
Oncologists debate whether TKI monotherapy has a place in renal cell carcinoma treatment after the CLEAR trial.
The Seattle Cancer Care Alliance expert discusses key takeaways from cohort a of the KEYTRUDA-427 study, evaluating pembrolizumab monotherapy in patients with clear cell renal cell carcinoma.
The Seattle Cancer Care Alliance Expert offered background on cohort A of the KEYNOTE-427 trial.
The Seattle Cancer Care Alliance Expert offered background on the first-line use of pembrolizumab monotherapy in advanced clear cell renal cell carcinoma.

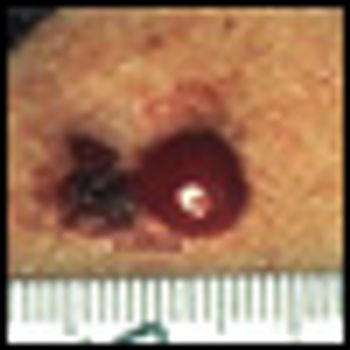
In this article, we summarize the systemic therapies now available for melanoma, with a focus on the recently approved agents for cutaneous melanoma; discuss important considerations in selecting a treatment from the available options; and highlight some of the promising investigational approaches for this disease.
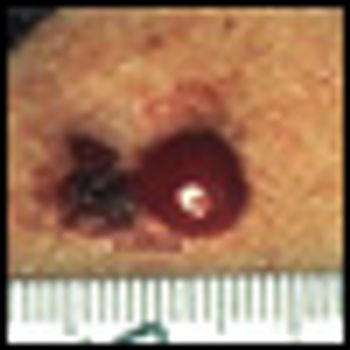
Metastatic melanoma continues to be a challenging disease to treat, with an estimated 8,420 related deaths in the United States in 2008.[1] The 10- year survival rate for patients with metastatic melanoma is less than 10%.[2] More than 3 decades after its initial approval by the US Food and Drug Administration (FDA) in 1975, dacarbazine continues to be the standard of care for most patients with this disease. High-dose interleukin-2 (HD IL-2 [Proleukin]), approved by the FDA in 1998 for metastatic melanoma, benefits a small subset of patients.