42 Transitional Lymphedema: Understanding the Temporal Dynamics Post-Axillary Surgery
Background
Lymphedema poses a significant challenge for patients with breast cancer who have undergone axillary lymph node dissection (ALND). Traditional techniques for lymphedema assessment, such as arm circumference measurement and bioimpedance spectroscopy (Lymphedema Index [L-Dex]), have been useful but limited in scope. One underexamined facet of this condition is its temporal characteristics—specifically, the period between surgery and the onset of lymphedema symptoms. Our study aims to elucidate the concept of transitional lymphedema, a term we propose to describe lymphedema occurring between 3 to 6 months after axillary surgery that would be resolved with longer follow-up.
Methods
A retrospective cohort study included patients with breast cancer undergoing ALND with Simplified Lymphatic Microsurgical Preventing Healing Approach (SLYMPHA) between January 2019 and June 2022 at a single institution. Patient demographics and treatment characteristics were collected. An L-Dex score outside the normal range (±10 L-Dex unit) or an increase of at least 10 L-Dex units above the patient’s baseline was considered abnormal.
Results
L-Dex Score at Each Postoperative Visit
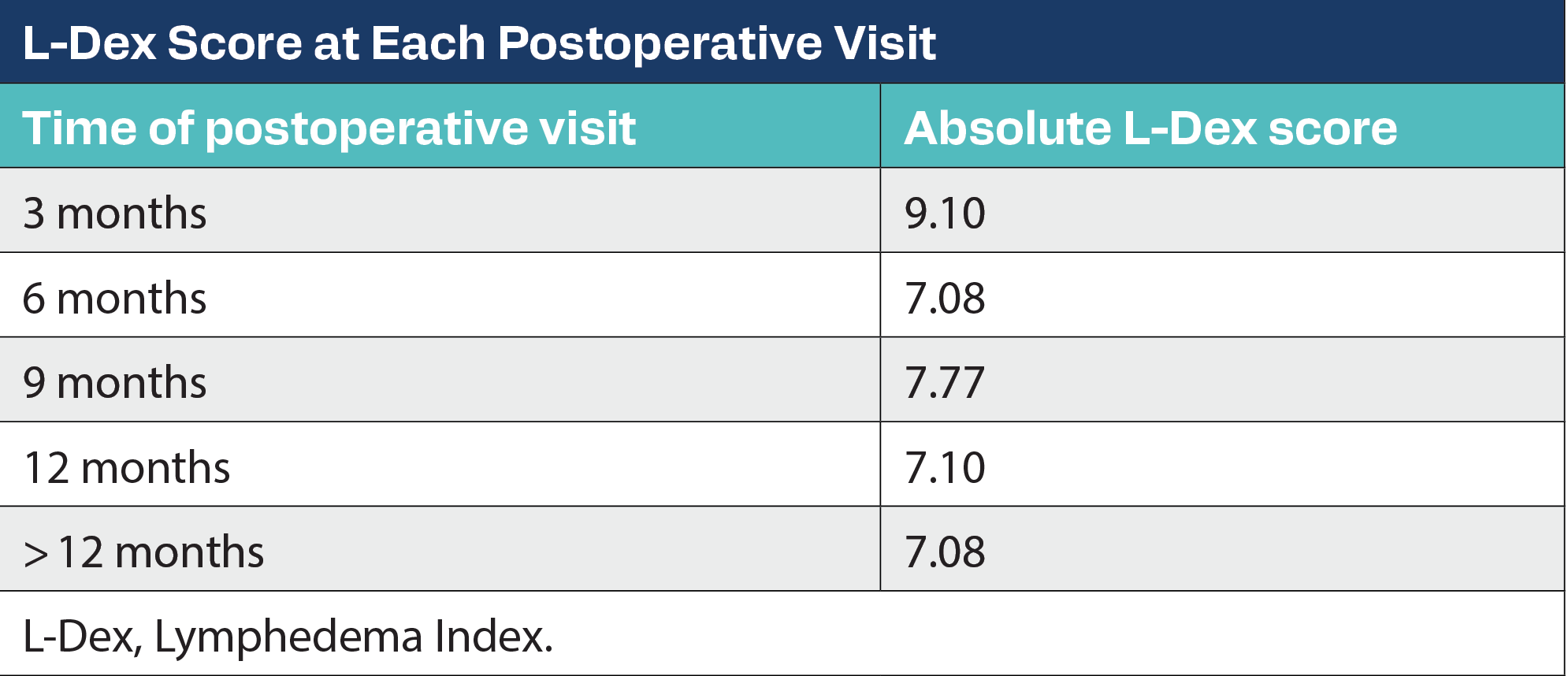
A total of 51 patients met the inclusion criteria, with a mean (SD) age of 56.8 (12.6) years and a mean (SD) body mass index (BMI) of 29.5 (7.2) kg/m2. A total of 41 patients (80.4%) received adjuvant radiation, and 41 patients (80.4%) received neoadjuvant chemotherapy. Of the 18 patients with abnormal L-Dex scores, an abnormal L-Dex developed in 5 patients (27.7%) at 3 months, 6 patients (33.3%) at 6 months, 3 patients (16.6%) at 9 months, and 4 patients (22.2%) at 12 months. There was a decrease in the mean absolute L-Dex score at each postoperative visit. When comparing the L-Dex difference from the baseline, it was lower at 12 months (4.67) compared with the 3-month (10.12) postoperative visit (CI, 0.1086-9.968; P = .0432). Additionally, 88.2% of patients who developed an abnormal L-Dex score at some time had adjuvant radiation compared with 76.4% of patients who never had an abnormal L-Dex reading; however, it was not significant. Of note, 52.17% of patients with BMI of at least 30 kg/m2 developed abnormal L-Dex scores compared with 22.2% of patients with a BMI below 30 kg/m2 (P = .02). From patients with at least 20 axillary lymph nodes removed, 45% developed abnormal L-Dex, whereas it was 28.5% when fewer than 20 lymph nodes were removed (P = .04).
Conclusions
Most increases in L-Dex scores seen in the first 6 postoperative months showed resolution after a follow-up of more than 12 months. Higher BMI (≥ 30 kg/m2) and removal of at least 20 axillary lymph nodes were associated with higher L-Dex measurements during postoperative follow-up visits.

Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.
The Proper Ways to Identify and Use ADCs in Breast Cancer Subtypes
June 29th 2025Deciding when to use immunotherapy and how to utilize antibody-drug conjugates are complicated processes that require multidisciplinary collaboration to ensure that all patients with breast cancer receive appropriate and efficient care.