- ONCOLOGY Vol 35, Issue 7
- Volume 35
- Issue 7
Combination Therapy With Immune Checkpoint Inhibitors in Urothelial Carcinoma: Current Data and Future Outlook
Until 5 years ago, systemic therapeutic options for urothelial carcinoma, the most common form of bladder cancer, had been limited to cisplatin-based regimens and taxanes. This article explores the current and future outlooks for combination therapy with IOs in urothelial carcinoma.
Introduction
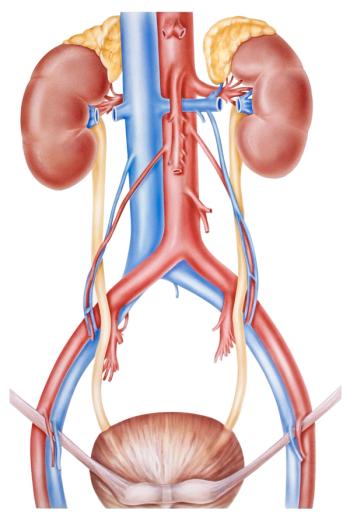
Bladder cancer is the sixth most common cancer in the United States, with an estimated 81,400 new cases in 2020. Although bladder cancer has 4 stages, for systemic treatment we recognize 3 clinical stages: non–muscle-invasive bladder cancer (NMIBC), muscle-invasive bladder cancer (MIBC), and locally advanced/metastatic urothelial carcinoma (mUC). Approximately 70% to 80% of patients present with NMIBC at diagnosis and have an excellent 5-year overall survival (OS) of 69.2% to 95.8%.1 About 10% to 15% of patients present with MIBC at the time of diagnosis and have about a 50% chance of progressing to metastatic disease.2 mUC accounts for 10% to 15% of all bladder cancers at diagnosis, with a 5-year OS for patients of fewer than 10% with platinum-based chemotherapy.
Oncology (Williston Park). 2021;35(7):410-420.
DOI: 10.46883/ONC.2021.3507.0410
1. mUC
Historically, mUC is considered a chemotherapy-sensitive disease with response rates of 50% to 60%.3-5 However, cisplatin-based regimens (eg, methotrexate/vinblastine/doxorubicin/cisplatin [MVAC]; gemcitabine/cisplatin) result in a high rate of complications, including nephrotoxicity, ototoxicity, neurotoxicity, and cardiotoxicity, and about half of patients are ineligible to receive cisplatin-based therapy due to renal insufficiency, poor performance status, or preexisting neurotoxicity and hearing loss. Median OS (OS) for patients with mUC is poor, at 13.8 to 14.8 months.5
In 2017, after promising results from the phase 2 KEYNOTE-052 (NCT02335424) and phase 2 IMvigor210 trials (NCT02108652), the FDA granted accelerated approval to 2 immune checkpoint inhibitors (ICIs), pembrolizumab and atezolizumab, as first-line treatment for patients with locally advanced or metastatic UC who were not eligible for platinum-based therapy.6-8 Both trials enrolled similar patients; they were cisplatin ineligible and treatment naïve in the metastatic setting. The results of both trials demonstrated comparable response rates of 23% to 29% (Table 1). In the KEYNOTE-052 trial, the median duration of response (DOR) was 30 months, with an OS of 11.3 months; in patients with a combined positive score of 10 or higher, the objective response rate (ORR) was 47% and median OS was 18.5 months. This was similar to that of patients with lymph node–only disease. In the 42% of patients with an ECOG performance status of 2 and in the 38% of patients who were older than 75 years, the response rates and overall outcomes were similar.7
Patients treated in the second-line setting have a poor prognosis, with a median OS of less than 6 months. Between 2016 and 2017, atezolizumab, nivolumab, avelumab, durvalumab, and pembrolizumab were approved by the FDA as second-line treatment for advanced or metastatic UC following the failure of platinum-based systemic treatment. This approval came after convincing data from the phase 2 IMvigor210,8 phase 2 CheckMate 275 (NCT02387996),9 phase 1 JAVELIN solid tumor (NCT01772004),10 phase 1/2 STUDY 1108 trial (NCT01693562),11 and phase 3 KEYNOTE-045 trials (NCT02256436).12 Table 2 describes the outcomes of these trials in second-line post-platinum therapy.
1.1 ICIs in combination with chemotherapy in mUC
Cytotoxic therapy can promote antitumor immunity by modifying the tumor-suppressive microenvironment composition. The release of “danger” molecules from tumor cells, such as calreticulin, polarizes dendritic cells toward a proinflammatory phenotype, thus increasing priming toward T helper 1 cells and away from regulatory T cells. Multiple lines of evidence suggest that immunotherapies combined with chemotherapy may deliver a greater potency than ICI monotherapy.13,14
To test this hypothesis, the phase 3 KEYNOTE-361 (NCT02853305) and phase 3 IMvigor130 (NCT02807636) trials randomized first-line patients with mUC who were cisplatin eligible to pembrolizumab or atezolizumab monotherapy; ICI in combination with chemotherapy; or chemotherapy alone. The primary end point for both was progression-free survival (PFS). In both studies, the ICI-only arm in patients with low PD-L1 tumors was ended early after an FDA alert in May 2018 warned of decreased survival in this group. In both trials, the primary end point was not reached. In KEYNOTE-361, the PFS in the pembrolizumab/chemotherapy combination arm was 8.3 months compared with 7.1 months in the chemotherapy-only arm (HR, 0.78; 95% CI, 0.65-0.93; P = .0033); OS was 17.0 vs 14.3 months, respectively (HR, 0.86; 95% CI, 0.72–1.02; P = .0407).15 In the IMvigor130 trial at a median follow-up of 11.8 months, median PFS was 8.2 months in the combination arm vs 6.3 months in the chemotherapy-only arm (HR, 0.82; 95% CI, 0.70-0.96; P = .007) and median OS was 16.0 vs 13.4 months, respectively (Table 3).16 The IMvigor130 and KEYNOTE-361 trials currently support chemotherapy as first-line therapy for platinum-eligible patients. When combined with chemotherapy, ICI does not appear to confer any additional benefit in ORR, PFS, or OS. Sequential therapy with chemotherapy then maintenance ICI is the current standard of care (SOC) based on the phase 3 JAVELIN 100 trial (NCT02603432), which demonstrated improvement in OS for avelumab vs placebo post chemotherapy in patients with stable disease or better response to first-line chemotherapy.17
The use of lower doses of chemotherapy to stimulate an immune response is also being investigated in a phase 2 trial (NCT02581982) in the second-line setting with low-dose paclitaxel and pembrolizumab. Data presented at the 2021 American Society of Clinical Oncology Genitourinary Annual Meeting (ASCO GU) reported a response rate of 33%. The 6-month PFS was 46.8% (95% CI, 27%-64.2%) and median OS was 11.7 months (95% CI, 8.7 to not reached). This preliminary result illustrates that the addition of a low dose of paclitaxel to pembrolizumab results in a favorable response and is tolerable. However, this should be confirmed in a phase 3 setting.18
1.2 Dual Immunotherapy in mUC
Combination therapy with both anti–PD-1/PD-L1 and anti–CTLA-4 agents has proven synergistic effects, and ipilimumab (Yervoy)/nivolumab has been approved in the treatment of melanoma, renal cell carcinoma, and microsatellite instability–high colon cancer. However, the combination has higher toxicity than monotherapy.19-21
There are three phase 3 trials studying immunotherapy oncology (IO) doublets (ie, an anti–PD-1/PD-L1 agent plus an anti–CTLA-4 agent) vs chemotherapy as first-line treatment for mUC in both platinum-eligible and -ineligible patients. Tremelimumab is a fully humanized immunoglobulin G2 monoclonal antibody against CTLA-4. The DANUBE trial (NCT 02516241) evaluated the efficacy in mUC of durvalumab vs durvalumab/tremelimumab, followed by durvalumab maintenance vs chemotherapy. The primary end points of the trial were PFS and OS of the durvalumab/tremelimumab combination vs SOC, stratifying for PD-L1 status. The trial did not meet its coprimary end points.22 In the high–PD-L1 population, OS was 14.4 months with durvalumab alone vs 12.1 months in the chemotherapy group (HR, 0.89; 95% CI, 0.71-1.11; P = .3). Overall OS was 15.1 months with durvalumab/tremelimumab vs 12.1 months with chemotherapy (HR, 0.85; 95% CI, 0.72-1.02; P = .075) in the intent-to-treat population.
Currently accruing trials include NILE (NCT03682068), which is investigating the combinations of durvalumab/tremelimumab/chemotherapy vs durvalumab/chemotherapy vs chemotherapy alone in the first-line setting; and CheckMate 901 (NCT03036098), which is studying nivolumab with either ipilimumab or chemotherapy vs chemotherapy alone, with primary end points of PFS and OS. Both trials are accruing patients who are cisplatin eligible and ineligible.
1.3 ICIs in combination with antibody-drug conjugates
EV, an antibody-drug conjugate (ADC) that targets Nectin-4, was approved in December 2019 based on the results of EV-201, a phase 2 study in patients with prior chemotherapy and ICI therapy.23 Approval was based on cohort 1, which included 125 patients who had progressed on both ICI and chemotherapy, with a confirmed response rate of 44% reported. The disease progression rate was 18%, translating to an 82% clinical benefit rate (CBR) in all subgroups. OS was 12.4 months (95% CI, 9.46-15.57). At ASCO GU 2021, the results of cohort 2 (cisplatin-ineligible patients with prior IO therapy) were reported; their ORR was 52%, including 20% who had a complete response (CR). Median PFS and median OS were 5.8 months and 14.7 months, respectively.24
EV-301 (NCT03474107), a randomized phase 3 trial evaluating EV vs chemotherapy alone in patients with previously treated mUC, demonstrated median OS of 12.9 months with EV vs 9.0 months with chemotherapy (HR, 0.70; 95% CI, 0.56-0.89; 1-sided P = .001) after a median follow-up of 11.1 months. The incidence of treatment-related adverse events (TRAEs) was 93.9% vs 91.8%, and the incidence of grade 3 or higher TRAEs was 51.4% vs 49.8%, in the EV and chemotherapy groups, respectively.25
In the phase 1/2 EV-103 trial which combined EV with pembrolizumab in cisplatin-ineligible patients in the first-line setting, the combination had an ORR of 73% and an additional 20% of patients experienced stable disease (disease control rate 93%). The results did not appear to be dependent on PD-L1 expression.26 This rate of high response to EV both as monotherapy and in combination with pembrolizumab is promising, and it has resulted in several ongoing trials including EV-302 (NCT04223856), an open-label, randomized phase 3 trial studying EV in combination with pembrolizumab vs chemotherapy alone in previously untreated locally advanced or metastatic UC.
Sacituzumab govitecan (Trodelvy) is another ADC targeting trophoblast cell surface antigen-2 (Trop-2) linked to SN38, a topoisomerase inhibitor, that has shown promising activity in the third-line setting. Trop-2 is a transmembrane calcium signal transducer that is highly expressed in many human epithelial malignancies.27 It regulates cancer growth, invasion, and metastasis by multiple signaling pathways.28 Recent data from cohort 1 of the phase 2 TROPHY-U-01 trial (NCT03547973) reported an ORR of 27% with sacituzumab govitecan in patients with mUC who were previously treated with chemotherapy and PD-1/PD-L1 therapy. CR was reported in 5% of patients, and 22% achieved partial response.29,30 Given the promising data from cohort 1, the response rate to and safety of sacituzumab govitecan combined with pembrolizumab will be assessed in cohort 3 patients who progressed after prior platinum-based therapies but have not received immunotherapy.
Additionally, the FDA has recently granted accelerated approval to sacituzumab govitecan for locally advanced or metastatic UC previously treated with platinum-based chemotherapy and immunotherapy.31 A phase 3 trial, TROPiCS-04 (NCT04527991), has also been initiated to compare sacituzumab govitecan with physician’s choice (single-agent taxane or vinflunine) in patients with metastatic or locally advanced unresectable UC who were treated with prior chemotherapy and ICI therapy.32
1.4 ICIs in combination with targeted therapy in mUC
Combinatorial regimens of ICI and targeted therapy can result in synergistic effects (by targeting complementary pathways), improve outcomes of immunotherapy (by sensitizing tumor cells and improving effector cells), and overcome resistance to checkpoint therapy. Some targeted therapies may directly modulate the immune response by attenuating the activities of specific immune cell populations that restrain cytotoxic T lymphocytes.33,34
Erdafitinib, an FGFR inhibitor, received accelerated approval from the FDA in 2019 as the first targeted drug for patients with either locally advanced mUC or mUC harboring the FGFR2/3 mutation or gene fusion (found in approximately 20% of patients with mUC). A recent study showed that inhibiting erdafitinib led to upregulation of BST2, a gene associated with activated interferon signaling and the immune system.35 Patients with FGFR mutations or fusions may have lower sensitivity to ICI.
Table 3 describes the current trials with erdafitinib and ICI combinations. An ongoing phase 1b/2 trial (NCT03473743) is studying the safety, tolerability, and efficacy of the combination of erdafitinib with cetrelimab, a PD-1 antibody, in cisplatin-ineligible patients with locally advanced or mUC harboring FGFR gene alterations.
The FORT-2 study (NCT03473756) is a phase 1b/2 trial studying the combination of atezolizumab with rogaratinib, an FGFR inhibitor, as first-line treatment in cisplatin-ineligible patients harboring the FGFR alteration, with primary end points of toxicity and PFS.
FIERCE-22 (NCT03123055) is a phase 1b/2 single-arm trial evaluating the combination of pembrolizumab with vofatamab, an FGFR3 inhibitor, in patients with platinum-refractory mUC. The combination was active in patients with both wild-type and mutated FGFR3, with an ORR of 29.6%.36
BISCAY was a novel biomarker-directed platform that sought to evaluate ICI in combination with targeted therapies in patients with platinum-refractory mUC. Combinations of durvalumab with AZD4547 (an FGFR inhibitor), olaparib (Lynparza; a PARP inhibitor), and vistusertib (a TORC inhibitor) were evaluated. Unfortunately, the overall response to durvalumab was not amplified by adding any of these targeted agents.37
The tryptophan catalytic enzyme IDO1 is an important immune regulatory protein; it can drive cancer immunosuppression by stimulating regulatory T cells and suppressing CD8 T effector cells, and it can be upregulated by anti–PD-1 agents. Linrodostat mesylate, an oral IDO1 inhibitor, has been evaluated in combination with nivolumab in the phase 1/2 advBC trial (NCT02658890) for patients with mUC who were not previously treated by ICIs, following 1 or more prior lines of therapy. Results included an ORR of 37% and a disease control rate of 56%.38
MARIO-275 (NCT03980041) is a randomized phase 2 trial evaluating the safety and efficacy of the PI3K-gamma inhibitor eganelisib combined with nivolumab in patients with mUC who have progressed on a platinum-based chemotherapy regimen but who are immunotherapy naïve. Eligible patients were randomized 2:1 to receive eganelisib in combination with nivolumab or placebo with nivolumab, stratified by the level of baseline circulating monocytic myeloid-derived suppressor cells (MDSCs). One of the mechanisms of PI3K-gamma is to maintain the immunosuppressive role of macrophages and MDSCs. Preliminary results showed that the primary end point, ORR, was higher in the eganelisib/nivolumab arm compared with the placebo/nivolumab arm in both the low monocytic MDSC subgroup (38.5% vs 23.1%, respectively) and the PD-L1 negative subgroup (26.1% vs 14.3%, respectively). TRAEs were more common in the eganelisib/nivolumab arm even after dose reduction.39
2. MIBC
The standard treatment for patients with MIBC is neoadjuvant chemotherapy followed by radical cystectomy with a recent meta-analysis showing an absolute OS benefit of 5%. Local recurrence was 30% to 54% with a 50% reduction in the risk of distant disease with neoadjuvant therapy followed by radical cystectomy.40,41 Pathological response is a surrogate for OS.42-44 However, as a result of cisplatin ineligibility (50%) or refusal to receive chemotherapy (30%), only about 20% of patients with MIBC are treated with cisplatin-based neoadjuvant chemotherapy.40
Due to the success of IO therapy in the metastatic setting, multiple trials of ICIs in the neoadjuvant setting for MIBC are currently accruing. The agents include ICI monotherapy and combinations of IO/chemotherapy and IO/targeted therapies.
Both the phase 2 PURE-01 (NCT02736266) and phase 2 ABACUS trials (NCT02662309) evaluating pembrolizumab and atezolizumab reported favorable pathological response rates in the neoadjuvant setting. Pathological CR (pCR) in the PURE-01 trial was 42% and an additional 12% patients were either pTa, Tis or pT1. PD-L1 expression was associated with higher pCR response.45 In the ABACUS trial, the pCR rate was 31%, with no significant correlation with PD-L1 expression.46 The pCR rates from the PURE-01 and ABACUS trials are similar to historic rates reported with neoadjuvant chemotherapy (38% with MVAC)42 and with fewer toxicities. Given these promising phase 2 data, ICI combination therapy is being investigated in the neoadjuvant setting.
2.1 Neoadjuvant dual immunotherapy with MIBC
NABUCCO (NCT03387761) is a single-arm phase 1b trial that studied the feasibility of preoperative ipilimumab plus nivolumab in MIBC, with 24 enrolled patients. Eleven patients (46%) achieved pCR (pT0N0) and 58% of patients were downstaged to noninvasive disease. The pCR rate was 73% in the PD-L1–positive group and 33% in the PD-L1–negative group (P = .15).47 Currently, a nonrandomized phase 2 study designed to evaluate neoadjuvant nivolumab vs nivolumab and ipilimumab in patients with MIBC who are ineligible for cisplatin-based chemotherapy (NCT03520491) is underway and still recruiting (Table 4).
The results of a pilot trial of the combination of durvalumab and tremelimumab as neoadjuvant therapy (NCT02812420) have been reported for cisplatin-ineligible patients with high-risk disease, defined as bulky tumors, variant histology, lymphovascular invasion, hydronephrosis, or high-grade upper tract disease.48,49 The primary end point was safety, and 21.4 % of patients had grade ≥ 3 immunotherapy-related toxicity; 37.5% of patients achieved pCR and 58.0% of patients downstaged to pT1 or less.48
The phase 2 DUTRENEO trial (NCT03472274) sought to evaluate tumor proinflammatory interferon-gamma tumor inflammation signature (TIS) to predict which patients might benefit from dual IO therapy (durvalumab/tremelimumab) vs chemotherapy as neoadjuvant therapy.50 Patients with cT2-4/or who were N+ stage and cisplatin eligible were classified as having “hot” or “cold” tumors according to TIS score determined by Nanostring technology.51 Patients with “hot” tumors were randomized to a cisplatin-based chemotherapy group or a combined chemotherapy/ICI group; patients with “cold” tumors were treated with cisplatin-based chemotherapy. The pCR rate was 68.8% in the “cold” chemotherapy group, 36.4% in the “hot” chemotherapy group, and 34.8% in the “hot” combined IO group. Tumors with higher PD-L1 expression predicted higher pCR rate only when treated with combined IO, not with chemotherapy.50 The AE profile of combined IO therapy seemed to be favorable compared with that of chemotherapy. However, the role of TIS score in immunotherapy selection is still unclear. Further study is required to validate this biomarker.
2.2 Neoadjuvant ICI/chemotherapy combination treatments in MIBC
Numerous clinical trials with ICI/chemotherapy combinations in the neoadjuvant setting are underway for MIBC (Table 4).The GU14-188 trial (NCT02365766) is a phase 1b/2 study evaluating neoadjuvant pembrolizumab with gemcitabine/cisplatin (GC) in cisplatin-eligible) and gemcitabine alone in cisplatin-ineligible patients with T2-4aN0M0 bladder cancer. The
primary end points were toxicity and pathologic non–muscle-invasive response rate (PaIR) (ie, ypT0, Tis, Ta, T1, and N0).52 A total of 42 patients were enrolled in the cisplatin-eligible cohort. With pembrolizumab/GC, the PaIR was 61% and the pCR rate was 44%. Neither correlated with the baseline PD-L1 score. At a median follow-up of 34.2 months, the estimated 36-month recurrence-free survival was 63% and OS was 82%. Cohort 2 of the GU14-188 trial was designed to study the tolerability and efficacy of neoadjuvant gemcitabine with pembrolizumab in cisplatin-ineligible patients with cT2-4aN0M0 MIBC, with PaIR as the primary end point. The interim results were similar to those of cohort 1; PaIR was 51.6% and the pCR rate was 45.2%, and the response rate was not related to the baseline PD-L1 score.53 Given that the current SOC is dose-dense MVAC, with a pCR rate of 38%,42 the results of GU14-188 suggest that the pembrolizumab/GC combination is feasible with manageable toxicity.
Another phase 2 trial (NCT02690558) recently reported a 36% pCR rate and PaIR of 56% with neoadjuvant pembrolizumab plus gemcitabine and a split dose of cisplatin in patients with clinical T2-4a N0/X M0 urothelial bladder cancer who were eligible for cisplatin.54
The BLASST-1 trial (NCT03294304) was a phase 2 study of neoadjuvant nivolumab with GC in patients with MIBC prior to radical cystectomy (RC). The primary end point was non–muscle invasive disease (ypT <1). Secondary end points were the safety of GC plus nivolumab and PFS at 2 years. A total of 41 patients were enrolled and 65.8% responded, including patients with cN1 disease. The pCR rate was 49% and response was not associated with PD-L1 status. The majority of AEs were from GC; immune-related AEs were seen in 3 patients but none required steroids.55
The SAKK 06/17 trial is another open-label, single-arm phase 2 study, enrolling 61 patients who had MIBC and were cisplatin eligible, cT2-T4a cN0-1. Four cycles of preoperative GC were administered, with durvalumab added starting with cycle 2. Durvalumab was then continued after surgery every 4 weeks for 10 cycles. The primary end point was event-free survival at 2 years, with PaIR as the secondary end point. Interim results showed that the PaIR rate was 60%, with 34% pCR in 53 patients who underwent surgery. Twelve percent and 2% of patients had grade 3 and grade 4 durvalumab-related AEs, respectively.56
NIAGARA (NCT03732677) is a randomized, open-label, global phase 3 trial of efficacy and safety of durvalumab in combination with GC as neoadjuvant therapy followed by durvalumab alone in the adjuvant setting in MIBC. The trial is still recruiting.57
The Aura trial (NCT03674424), currently recruiting, is an open-label, interventional, randomized phase 2 study investigating the safety and efficacy of avelumab in combination with chemotherapy in the adjuvant setting in patients with MIBC, both cisplatin eligible and ineligible.
2.4 Neoadjuvant ICIs in combination with targeted therapy in MIBC
Olaparib inhibits the DNA repair enzyme PARP and has been approved in ovarian, breast, and prostate cancer treatment. It has been hypothesized that PARP inhibitors can augment the tumor mutational burden, making bladder cancer more immunogenic by increasing neoantigen production and upregulating PD-L1 expression.58 The NEODURVARIB trial (NCT03534492) was a single-arm phase 2 study designed to assess the impact of neoadjuvant treatment with the combination of durvalumab plus olaparib in patients with resectable MIBC (cT2-T4a). Six to 8 weeks prior to planned cystectomy, patients received durvalumab 1500 mg intravenously every 4 weeks for up to 2 months and olaparib 300 mg twice a day orally for up to 56 days. Preliminary data showed that 10 patients (50%) had a pCR, which was very promising. However, 3 patients developed grade 4 AEs including wound evisceration, hemorrhage, and septic shock.58
Cabozantinib (Cabometyx) is a small molecule tyrosine kinase inhibitor (TKI) targeting c-Met, VEGFR2, AXL, and RET. Cabozantinib in combination with atezolizumab resulted in favorable responses in patients with mUC in the phase 1b COSMIC-021 trial (NCT03170960).59 Currently, this combination is being studied in the adjuvant setting. The ABATE trial (NCT04289779), currently recruiting, is a single-arm, open-label phase 2 study investigating the efficacy of cabozantinib and atezolizumab in patients with resectable MIBC who are ineligible for or decline cisplatin-based therapy. In this trial, atezolizumab 1200 mg is given every 3 weeks along with cabozantinib 40 mg daily. Each cycle is 21 days, and 3 cycles will be given before RC.
The promising results from the combination of linrodostat, the IDO1 inhibitor, and nivolumab in the mUC setting have led to the current study of linrodostat in the ENERGIZE trial (NCT03661320), a randomized, 3-arm phase 3 trial of neoadjuvant chemotherapy alone (arm A) or chemotherapy plus nivolumab (arm B) or chemotherapy plus nivolumab with linrodostat (arm C) for cisplatin-eligible patients with MIBC. The trial was designed to evaluate and compare the efficacy and safety of this regimen followed by adjuvant nivolumab alone (arm B) or nivolumab and linrodostat (arm C).60
2.5 Neoadjuvant ICIs with ADCs
The ADC EV was approved in December 2019 based on the promising results of a phase 2 study in the metastatic setting. Consequently, 2 open-label, randomized phase 3 trials involving EV in the neoadjuvant setting opened and are underway. These are MK-3475-905/KEYNOTE-905/EV-303 (NCT03924895), which will evaluate perioperative pembrolizumab vs perioperative EV in combination with pembrolizumab vs cystectomy alone in cisplatin-ineligible patients with MIBC; and MK-3475-B15/KEYNOTE-B15/EV-304 (NCT04700124), which evaluates perioperative EV in combination with pembrolizumab vs neoadjuvant chemotherapy in cisplatin-eligible patients with MIBC (Table 5).
In response to the promising data from TROPHY-U-01, there is a planned phase 2 trial evaluating neoadjuvant sacituzumab govitecan alone or in combination with pembrolizumab before RC (SURE trial).61
3. High-risk NMIBC
Approximately 70% of patients present with NMIBC such as pTa (70-75%), carcinoma in situ (CIS; 10%), and pT1 (15%) disease. Patients are risk stratified as low, intermediate, and high risk depending on pathological stage, grade, variant histology, size, and focality. Treatment and surveillance is based on risk stratification following transurethral resection of the bladder tumor and intravesical therapy with BCG and/or chemotherapy. Patients who are BCG unresponsive, candidates for early cystectomy, and at risk for progression to MIBC are the focus of investigational studies. BCG-unresponsive patients include those with refractory and BCG-relapsing cases; these are defined as persistent high-grade disease at 6 months despite adequate treatment and those with recurrence of high-grade disease after achieving a disease-free state at 6 months after adequate BCG, respectively.62
In January 2020, the FDA approved pembrolizumab based on the data showing that cohort A of KEYNOTE-057 (NCT02625961) demonstrated a 40.6% CR at 3 months, with a median DOR of 16.2 months.63 SWOG 1605 (NCT02844816) showed atezolizumab provided a similar response in patients with BCG-unresponsive high-risk NMIBC. The CR rate was 41.1% (95% CI, 29.7%-53.2%) at 3 months and 26.0% (95% CI, 16.5%- 37.6%) at 6 months.64 Trials are currently ongoing with durvalumab monotherapy in BCG-refractory CIS of the bladder (NCT02901548) and in NMIBC (NCT03759496).
3.1 ICIs in combination with BCG in high-risk NMIBC
The possible roles of immune checkpoint signaling in BCG-resistant NMIBC65,66 and the promising data of ICI monotherapies64,67 suggest that combining ICIs with BCG therapy may increase the response rate. Several randomized, open-label trials are currently ongoing, including KEYNOTE-676 (NCT03711032), a phase 3 study of BCG with or without pembrolizumab in patients with high-risk NMIBC68; ALBAN (NCT03799835), a phase 3 trial evaluating the efficacy of atezolizumab in combination with 1-year BCG bladder instillation in BCG-naïve, high-risk NMIBC; POTOMAC (NCT03528694), a phase 3 trial investigating durvalumab and BCG vs BCG alone in high-risk, BCG-naïve NMIBC; and CheckMate 9UT (NCT03519256), a phase 2 study of nivolumab monotherapy, nivolumab plus linrodostat mesylate, or nivolumab plus BCG in BCG-unresponsive, high-risk NMIBC. We await the results of these still-accruing trials.
4. Discussion
The emerging data for ICI combinations in bladder cancer are exciting, with the potential to change the therapeutic landscape for all patients with this disease. Up to 50% of patients with mUC are platinum ineligible or decline chemotherapy in the first-line setting, and ICI monotherapy has allowed these patients to receive systemic therapy; some have achieved a durable response with lower toxicity. This is tempered by the finding that patients with tumors with low or no PD-L1 expression might not benefit, and for platinum-eligible patients, chemotherapy remains the SOC. In the second-line setting, ICIs have demonstrated survival benefit over chemotherapy. We now have EV, sacituzumab govitecan, and erdafitinib to be used in the third- or fourth-line setting depending on FGFR2/3 mutational status and other clinical factors such as patient preference and toxicity profile.
As outlined in this paper, the development of regimens that combine ICIs with other IO drugs (eg, anti–CTL-4 agents), chemotherapy (including ADCs), targeted therapy (eg, FGFR inhibitors, PARP inhibitors, multitargeted TKIs), and immune suppressors to overcome ICI resistance (eg, IDO1 inhibitors) is ongoing. The most promising regimen to date is the combination of EV with pembrolizumab, with a response rate of more than 70% and a CBR of 90% in patients who are cisplatin ineligible, regardless of PD-L1 status. This regimen is now being compared with chemotherapy in the first-line setting in platinum-eligible patients and in the muscle-invasive setting.
In the muscle-invasive setting, the response rates to anti-PD-1/L1 as single agents when combined with other IO drugs (eg, anti–CTLA-4 agents), or with targeted therapy and chemotherapy, all appear to achieve pCR and pathological non–muscle-invasive rates that compare favorably with historical controls. If confirmed in larger randomized trials, these results will give patients who have not been able to receive chemotherapy in this setting an opportunity to receive therapy. The results of the CheckMate 274 trial (NCT02632409) show disease-free survival benefit in the adjuvant setting with nivolumab in patients with and without prior neoadjuvant therapy who demonstrate high-risk pathological features for recurrence. Again, the goal here is the ability to expand therapeutic options for patients, which will hopefully translate to improvement in OS with less toxicity. An additional advantage of neoadjuvant therapy is the ability to include biomarker analysis to help predict which patients might benefit. Beyond PD-L1, other predictive and prognostic biomarkers need to be investigated
ICIs are tools in the spectrum of treatments being investigated to improve outcomes in high-risk NMIBC.69 Novel intravesical therapies—including recombinant adenovirus gene transfer vector; oportuzumab monatox (Vicinium; a recombinant fusion protein drug consisting of an epithelial cell adhesion molecule–specific antibody fragment linked to a pseudomonas exotoxin A)70; and combination therapy along with BCG in the earlier setting—can potentially reduce progression to muscle-invasive disease and to recurrent high-risk disease, as well as reduce the need for early cystectomy.
There are indeed a wealth of agents and trials, but the meaningful end points and outcomes of OS, patient-reported quality of life, and pathological response rates, depending on clinical stage, remain critical to determining the best treatment options for our patients.
Financial Disclosure: JV receives research funding at her institution for clinical trials from Merck, Bristol Meyers Squibb, Genentech, Astellas, Seattle Genetics, Astra Zeneca.
CONFLICTS OF INTEREST: JV serves on advisory boards for AstraZeneca, Bristol Meyers Squibb, and Seattle Genetics
REFERENCES
1.Cancer stat facts: bladder cancer. National Cancer Institute: Surveillance, Epidemiology, and End Results Program. Accessed November 16, 2020. https://seer.cancer.gov/statfacts/html/urinb.html
2.Chul Park J, Citrin DE, Agarwal PK, Apolo AB. Multimodal management of muscle-invasive bladder cancer. Curr Probl Cancer. 2014;38(3):80-108. doi:10.1016/j.currproblcancer.2014.06.001
3.Bellmunt J, von der Maase H, Mead GM, et al. Randomized phase III study comparing paclitaxel/cisplatin/gemcitabine and gemcitabine/cisplatin in patients with locally advanced or metastatic urothelial cancer without prior systemic therapy: EORTC Intergroup Study 30987. J Clin Oncol. 2012;30(10):1107-1113. doi:10.1200/jco.2011.38.6979
4.von der Maase H, Sengelov L, Roberts JT, et al. Long-term survival results of a randomized trial comparing gemcitabine plus cisplatin, with methotrexate, vinblastine, doxorubicin, plus cisplatin in patients with bladder cancer. J Clin Oncol. 2005;23(21):4602-4608. doi:10.1200/jco.2005.07.757
5.von der Maase H, Hansen SW, Roberts JT, et al. Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. J Clin Oncol. 2000;18(17):3068-3077. doi:10.1200/jco.2000.18.17.3068
6.Vuky J, Balar AV, Castellano D, et al. Long-term outcomes in KEYNOTE-052: phase II study investigating first-line pembrolizumab in cisplatin-ineligible patients with locally advanced or metastatic urothelial cancer. J Clin Oncol. 2020;38(23):2658-2666. doi:10.1200/jco.19.01213
7.Grivas P, Plimack ER, Balar AV, et al. Pembrolizumab as first-line therapy in cisplatin-ineligible advanced urothelial cancer (KEYNOTE-052): outcomes in older patients by age and performance status. Eur Urol Oncol. 2020;3(3):351-359. doi:10.1016/j.euo.2020.02.009
8.Balar AV, Galsky MD, Rosenberg JE, et al; IMvigor210 Study Group. Atezolizumab as first-line treatment in cisplatin-ineligible patients with locally advanced and metastatic urothelial carcinoma: a single-arm, multicentre, phase 2 trial. Lancet. 2017;389(10064):67-76. doi:10.1016/s0140-6736(16)32455-2
9.Sharma P, Retz M, Siefker-Radtke A, et al. Nivolumab in metastatic urothelial carcinoma after platinum therapy (CheckMate 275): a multicentre, single-arm, phase 2 trial. Lancet Oncol. 2017;18(3):312-322. doi:10.1016/s1470-2045(17)30065-7
10.Patel MR, Ellerton J, Infante JR, et al. Avelumab in metastatic urothelial carcinoma after platinum failure (JAVELIN Solid Tumor): pooled results from two expansion cohorts of an open-label, phase 1 trial. Lancet Oncol. 2018;19(1):51-64. doi:10.1016/s1470-2045(17)30900-2
11.Powles T, O’Donnell PH, Massard C, et al. Efficacy and safety of durvalumab in locally advanced or metastatic urothelial carcinoma: updated results from a phase 1/2 open-label study. JAMA Oncol. 2017;3(9):e172411. doi:10.1001/jamaoncol.2017.2411
12.Bellmunt J, de Wit R, Vaughn DJ, et al; KEYNOTE-045 Investigators. Pembrolizumab as second-line therapy for advanced urothelial carcinoma. N Engl J Med. 2017;376(11):1015-1026. doi:10.1056/NEJMoa1613683
13.Opzoomer JW, Sosnowska D, Anstee JE, Spicer JF, Arnold JN. Cytotoxic chemotherapy as an immune stimulus: a molecular perspective on turning up the immunological heat on cancer. Front Immunol. 2019;10:1654. doi:10.3389/fimmu.2019.01654
14.Shiao SL, Preethi Ganesan A, Rugo HS, Coussens LM. Immune microenvironments in solid tumors: new targets for therapy. Genes Dev. 2011;25(24):2559-2572. doi:10.1101/gad.169029.111
15.Alva A, Csőszi T, Ozguroglu M, et al. LBA23 Pembrolizumab (P) combined with chemotherapy (C) vs C alone as first-line (1L) therapy for advanced urothelial carcinoma (UC): KEYNOTE-361. Ann Oncol. 2020;31(Suppl 4):S1155. doi:10.1016/j.annonc.2020.08.2252
16.Galsky MD, Arranz Arija JÁ, Bamias A, et al; IMvigor130 Study Group. Atezolizumab with or without chemotherapy in metastatic urothelial cancer (IMvigor130): a multicentre, randomised, placebo-controlled phase 3 trial. Lancet. 2020;395(10236):1547-1557. doi:10.1016/s0140-6736(20)30230-0
17.Powles T, Park SH, Voog E, et al. Avelumab maintenance therapy for advanced or metastatic urothelial carcinoma. N Engl J Med. 2020;383(13):1218-1230. doi:10.1056/NEJMoa2002788
18.Bitting RL, Vile DC, Tooze JA, et al. Single-arm phase II study of low-dose paclitaxel and pembrolizumab in platinum-refractory metastatic urothelial carcinoma (UC). J Clin Oncol. 2021;39(Suppl 6):abstr 433. doi:10.1200/JCO.2021.39.6_suppl.433
19.Wolchok JD, Chiarion-Sileni V, Gonzalez R, et al. Overall survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 2017;377(14):1345-1356. doi:10.1056/NEJMoa1709684
20.Motzer RJ, Tannir NM, McDermott DF, et al; CheckMate 214 Investigators. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N Engl J Med. 2018;378(14):1277-1290. doi:10.1056/NEJMoa1712126
21.Overman MJ, Lonardi S, Wong KYM, et al. Durable clinical benefit with nivolumab plus ipilimumab in DNA mismatch repair-deficient/microsatellite instability-high metastatic colorectal Cancer. J Clin Oncol. 2018;36(8):773-779. doi:10.1200/jco.2017.76.9901
22.Powles TB, van der Heijden MS, Castellano Gauna D, et al. A phase III, randomized, open-label study of first-line durvalumab (D) with or without tremelimumab (T) vs standard of care chemotherapy in patients with unresectable, locally advanced or metastatic urothelial carcinoma (DANUBE). Ann Oncol. 2020;31(Suppl 4):S550. doi:10.1016/annonc/annonc274
23.Rosenberg JE, O’Donnell PH, Balar AV, et al. Pivotal trial of enfortumab vedotin in urothelial carcinoma after platinum and anti-programmed death 1/programmed death ligand 1 therapy. J Clin Oncol. 2019;37(29):2592-2600. doi:10.1200/jco.19.01140
24.Balar AV, McGregor BA, Rosenberg JE, et al. EV-201 cohort 2: enfortumab vedotin in cisplatin-ineligible patients with locally advanced or metastatic urothelial cancer who received prior PD-1/PD-L1 inhibitors. J Clin Oncol. 2021;39(Suppl 6):abstr 394. doi:10.1200/JCO.2021.39.6_suppl.394
25.Powles T, Rosenberg JE, Sonpavde GP, et al. Enfortumab vedotin in previously treated advanced urothelial carcinoma. N Engl J Med. 2021;384(12):1125-1135. doi:10.1056/NEJMoa2035807
26.Rosenberg JE, Flaig TW, Friedlander TW, et al. Study EV-103: preliminary durability results of enfortumab vedotin plus pembrolizumab for locally advanced or metastatic urothelial carcinoma. J Clin Oncol. 2020;38(Suppl 6):abstr 441. doi:10.1200/JCO.2020.38.6_suppl.441
27.Bardia A, Messersmith WA, Kio EA, et al. Sacituzumab govitecan, a Trop-2-directed antibody-drug conjugate, for patients with epithelial cancer: final safety and efficacy results from the phase I/II IMMU-132-01 basket trial. Ann Oncol. 2021;32(6):746-756. doi:10.1016/j.annonc.2021.03.005
28.Goldenberg DM, Stein R, Sharkey RM. The emergence of trophoblast cell-surface antigen 2 (TROP-2) as a novel cancer target. Oncotarget. 2018;9(48):28989-29006. doi:10.18632/oncotarget.25615
29.Tagawa ST, Balar AV, Petrylak DP, et al. TROPHY-U-01: a phase II open-label study of sacituzumab govitecan in patients with metastatic urothelial carcinoma progressing after platinum-based chemotherapy and checkpoint inhibitors. J Clin Oncol. Published online April 30, 2021. doi:10.1200/jco.20.03489
30.Loriot Y, Balar AV, Petrylak DP, et al. TROPHY-U-01 cohort 1 final results: a phase II study of sacituzumab govitecan (SG) in metastatic urothelial cancer (mUC) that has progressed after platinum (PLT) and checkpoint inhibitors (CPI). Ann Oncol. 2020;31(Suppl 4): S1142-S1215. 101016/annonc/annonc325.
31.FDA grants accelerated approval to sacituzumab govitecan for advanced urothelial cancer. FDA. April 13, 2021. Accessed June 2, 2021. https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-sacituzumab-govitecan-advanced-urothelial-cancer
32.Grivas P, Tagawa ST, Bellmunt J, et al. TROPiCS-04: study of sacituzumab govitecan in metastatic or locally advanced unresectable urothelial cancer that has progressed after platinum and checkpoint inhibitor therapy. J Clin Oncol. 2021;39(Suppl 6):abstr TPS498. doi:10.1200/JCO.2021.39.6_suppl.TPS498
33.Hu-Lieskovan S, Robert L, Homet Moreno B, Ribas A. Combining targeted therapy with immunotherapy in BRAF-mutant melanoma: promise and challenges. J Clin Oncol. 2014;32(21):2248-2254. doi:10.1200/jco.2013.52.1377
34.Vanneman M, Dranoff G. Combining immunotherapy and targeted therapies in cancer treatment. Nat Rev Cancer. 2012;12(4):237-251. doi:10.1038/nrc3237
35.Robinson BD, Vlachostergios PJ, Bhinder B, et al. Upper tract urothelial carcinoma has a luminal-papillary T-cell depleted contexture and activated FGFR3 signaling. Nat Commun. 2019;10(1):2977. doi:10.1038/s41467-019-10873-y
36.Siefker-Radtke AO, Lugowska I, Tupikowski K, et al. 917P - clinical activity of vofatamab (V), an FGFR3 selective antibody in combination with pembrolizumab (P) in metastatic urothelial carcinoma (mUC), updated interim analysis of FIERCE-22. Ann Oncol. 2019;30(Suppl 5):v365. doi:10.1093/annonc/mdz249.016
37.Powles T, Balar A, Gravis G, et al. 902O - an adaptive, biomarker directed platform study in metastatic urothelial cancer (BISCAY) with durvalumab in combination with targeted therapies. Ann Oncol. 2019;30(Suppl 5):v356-v357. doi:10.1093/annonc/mdz249.001
38.Luke JJ, Tabernero J, Joshua A, et al. BMS-986205, an indoleamine 2, 3-dioxygenase 1 inhibitor (IDO1i), in combination with nivolumab (nivo): updated safety across all tumor cohorts and efficacy in advanced bladder cancer (advBC). J Clin Oncol. 2019;37(Suppl 7):abstr 358. doi:10.1200/JCO.2019.37.7_suppl.358
39.Tomczak P, Popovic L, Barthelemy P, et al. Preliminary analysis of a phase II, multicenter, randomized, active-control study to evaluate the efficacy and safety of eganelisib (IPI 549) in combination with nivolumab compared to nivolumab monotherapy in patients with advanced urothelial carcinoma. J Clin Oncol. 2021;39(Suppl 6):abstr 436. doi:10.1200/JCO.2021.39.6_suppl.436
40.Hanna N, Trinh QD, Seisen T, et al. Effectiveness of neoadjuvant chemotherapy for muscle-invasive bladder cancer in the current real world setting in the USA. Eur Urol Oncol. 2018;1(1):83-90. doi:10.1016/j.euo.2018.03.001
41.Meeks JJ, Bellmunt J, Bochner BH, et al. A systematic review of neoadjuvant and adjuvant chemotherapy for muscle-invasive bladder cancer. Eur Urol. 2012;62(3):523-533. doi:10.1016/j.eururo.2012.05.048
42.Barton Grossman H, Natale RB, Tangen CM, et al. Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. N Engl J Med. 2003;349(9):859-866. doi:10.1056/NEJMoa022148
43.Petrelli F, Coinu A, Cabiddu M, Ghilardi M, Vavassori I, Barni S. Correlation of pathologic complete response with survival after neoadjuvant chemotherapy in bladder cancer treated with cystectomy: a meta-analysis. Eur Urol. 2014;65(2):350-357. doi:10.1016/j.eururo.2013.06.049
44.Goel S, Sinha RJ, Bhaskar V, Aeron R, Sharma A, Singh V. Role of gemcitabine and cisplatin as neoadjuvant chemotherapy in muscle invasive bladder cancer: experience over the last decade. Asian J Urol. 2019;6(3):222-229. doi:10.1016/j.ajur.2018.06.006
45.Necchi A, Anichini A, Raggi D, et al. Pembrolizumab as neoadjuvant therapy before radical cystectomy in patients with muscle-invasive urothelial bladder carcinoma (PURE-01): an open-label, single-arm, phase II study. J Clin Oncol. 2018;36(34):3353-3360. doi:10.1200/jco.18.01148
46.Powles T, Kockx M, Rodriguez-Vida A, et al. Clinical efficacy and biomarker analysis of neoadjuvant atezolizumab in operable urothelial carcinoma in the ABACUS trial. Nat Med. 2019;25(11):1706-1714. doi:10.1038/s41591-019-0628-7
47.van Dijk N, Gil-Jimenez A, Silina K, et al. Preoperative ipilimumab plus nivolumab in locoregionally advanced urothelial cancer: the NABUCCO trial. Nat Med. 2020;26(12):1839-1844. doi:10.1038/s41591-020-1085-z
48.Gao J, Navai N, Alhalabi O, et al. Neoadjuvant PD-L1 plus CTLA-4 blockade in patients with cisplatin-ineligible operable high-risk urothelial carcinoma. Nat Med. 2020;26(12)1845-1851. doi:10.1038/s41591-020-1086-y
49.Culp SH, Dickstein RJ, Grossman HB, et al. Refining patient selection for neoadjuvant chemotherapy before radical cystectomy. J Urol. 2014;191(1):40-47. doi:10.1016/j.juro.2013.07.061
50.Grande E, Guerrero F, Puente J, et al. DUTRENEO trial: a randomized phase II trial of DUrvalumab and TREmelimumab versus chemotherapy as a NEOadjuvant approach to muscle-invasive urothelial bladder cancer (MIBC) patients (pts) prospectively selected by an interferon (INF)-gamma immune signature. J Clin Oncol. 2020;38(Suppl 15):abstr 5012. doi:10.1200/JCO.2020.38.15_suppl.5012
51.Danaher P, Warren S, Lu R, et al. Pan-cancer adaptive immune resistance as defined by the Tumor Inflammation Signature (TIS): results from The Cancer Genome Atlas (TCGA). J Immunother Cancer. 2018;6(1):63. doi:10.1186/s40425-018-0367-1
52.Hoimes CJ, Adra N, Fleming MT, et al. Phase Ib/II neoadjuvant (N-) pembrolizumab (P) and chemotherapy for locally advanced urothelial cancer (laUC): final results from the cisplatin (C)-eligible cohort of HCRN GU14-188. J Clin Oncol. 2020;38(Suppl 15):abstr 5047. doi:10.1200/JCO.2020.38.15_suppl.5047
53.Kaimakliotis HZ, Adra N, Kelly WK, et al. Phase II neoadjuvant (N-) gemcitabine (G) and pembrolizumab (P) for locally advanced urothelial cancer (laUC): interim results from the cisplatin (C)-ineligible cohort of GU14-188. J Clin Oncol. 2020;38(Suppl 15):abstr 5019. doi:10.1200/JCO.2020.38.15_suppl.5019
54.Rose TL, Harrison MR, Deal AM, et al. Phase II study of gemcitabine and split-dose cisplatin plus pembrolizumab as neoadjuvant therapy prior to radical cystectomy (RC) in patients with muscle-invasive bladder cancer (MIBC). J Clin Oncol. 2021;39(Suppl 6):abstr 396. doi:10.1200/JCO.2021.39.6_suppl.396
55.Gupta S, Sonpavde G, Weight CJ, et al. Results from BLASST-1 (Bladder Cancer Signal Seeking Trial) of nivolumab, gemcitabine, and cisplatin in muscle invasive bladder cancer (MIBC) undergoing cystectomy. J Clin Oncol. 2020;38(Suppl 6):abstr 439. doi:10.1200/JCO.2020.38.6_suppl.439
56.Cathomas R, Rothschild S, Hayoz S, et al. Safety and efficacy of perioperative cisplatin/gemcitabine (cis/gem) and durvalumab (durva) for operable muscle-invasive urothelial carcinoma (MIUC): SAKK 06/17. J Clin Oncol. 2021;39(Suppl 6):abstr 430. doi:10.1200/JCO.2021.39.6_suppl.430
57.Powles T, Meeks JJ, Galsky MD, et al. A phase III, randomized, open label, multicenter, global study of efficacy and safety of durvalumab in combination with gemcitabine+cisplatin (G+C) for neoadjuvant treatment followed by durvalumab alone for adjuvant treatment in muscle-invasive bladder cancer (MIBC) (NIAGARA). J Clin Oncol. 2019;37(Suppl 15):abstr TPS4592. doi:10.1200/JCO.2019.37.15_suppl.TPS4592
58.Rodriguez-Moreno JF, de Velasco G, Alvarez-Fernandez C, et al. 761P Impact of the combination of durvalumab (MEDI4736) plus olaparib (AZD2281) administered prior to surgery in the molecular profile of resectable urothelial bladder cancer. NEODURVARIB trial. Ann Oncol. 2020;31(Suppl 4):S589. doi:10.1016/j.annonc.2020.08.833
59.Pal SK, Agarwal N, Loriot Y, et al. Cabozantinib in combination with atezolizumab in urothelial carcinoma previously treated with platinum-containing chemotherapy: results from cohort 2 of the COSMIC-021 study. J Clin Oncol. 2020;38(Suppl 15):abstr 5013. doi:10.1200/JCO.2020.38.15_suppl.5013
60.Sonpavde G, Necchi A, Gupta S, et al. ENERGIZE: a phase III study of neoadjuvant chemotherapy alone or with nivolumab with/without linrodostat mesylate for muscle-invasive bladder cancer. Future Oncol. 2020;16(2):4359-4368. doi:10.2217/fon-2019-0611
61.Necchi A, Raggi D, Bandini M, et al. SURE: an open label, sequential-arm, phase II study of neoadjuvant sacituzumab govitecan (SG), and SG plus pembrolizumab (pembro) before radical cystectomy, for patients with muscle-invasive bladder cancer (MIBC) who cannot receive or refuse cisplatin-based chemotherapy. J Clin Oncol. 2021;39(Suppl 6):abstr TPS506. doi:10.1200/JCO.2021.39.6_suppl.TPS56
62.Kamat AM, Sylvester RJ, Böhle A, et al. Definitions, end points, and clinical trial designs for non-muscle-invasive bladder cancer: recommendations from the International Bladder Cancer Group. J Clin Oncol. 2016;34(16):1935-1944. doi:10.1200/jco.2015.64.4070
63.Vasant Balar A, Kamat AM, Kulkarni GS, et al. Pembrolizumab (pembro) for the treatment of patients with Bacillus Calmette-Guérin (BCG) unresponsive, high-risk (HR) non–muscle-invasive bladder cancer (NMIBC): over two years follow-up of KEYNOTE-057. J Clin Oncol. 2020;38(Suppl 15):abstr 5041. doi:10.1200/JCO.2020.38.15_suppl.5041
64.Black PC, Tangen C, Singh P, et al. Phase II trial of atezolizumab in BCG-unresponsive non-muscle invasive bladder cancer: SWOG S1605 (NCT #02844816). J Clin Oncol. 2020;38(Suppl 15):abstr 5022. doi:10.1200/JCO.2020.38.15_suppl.5022
65.Nakanishi J, Wada Y, Matsumoto K, Azuma M, Kikuchi K, Ueda S. Overexpression of B7-H1 (PD-L1) significantly associates with tumor grade and postoperative prognosis in human urothelial cancers. Cancer Immunol Immunother. 2007;56(8):1173-1182. doi:10.1007/s00262-006-0266-z
66.Hashizume A, Umemoto S, Yokose T, et al. Enhanced expression of PD-L1 in non-muscle-invasive bladder cancer after treatment with Bacillus Calmette-Guerin. Oncotarget. 2018;9(75):34066-34078. doi:10.18632/oncotarget.26122
67.Vasant Balar A, Kulkarni GS, Uchio EM, et al. KEYNOTE 057: phase II trial of pembrolizumab (pembro) for patients (pts) with high-risk (HR) nonmuscle invasive bladder cancer (NMIBC) unresponsive to bacillus calmette-guérin (BCG). J Clin Oncol. 2019;37(Suppl 7):abstr 350. doi:10.1200/JCO.2019.37.7_suppl.350
68.Kamat AM, Shore N, Hahn N, et al. KEYNOTE-676: phase III study of BCG and pembrolizumab for persistent/recurrent high-risk NMIBC. Future Oncol. 2020;16(10):507-516. doi:10.2217/fon-2019-0817
69.Albisinni S, Martinez Chanza N, Aoun F, et al. Immune checkpoint inhibitors for BCG-resistant NMIBC: the dawn of a new era. Minerva Urol Nefrol. Published online March 29, 2021. doi:10.23736/s2724-6051.21.04309-5
70.Shore N, O’Donnell M, Keane T, et al. PD03 Phase 3 results of vicinium in BCG-unresponsive non-muscle invasive bladder cancer. J Urol. 2020;203(Suppl 4):e72-e72. doi:10.1097/JU.0000000000000823.02
Articles in this issue
over 4 years ago
Clinical Trials in Progress: GOZILAover 4 years ago
Profilin 1 Protein and Its Implications for Cancersover 4 years ago
Advanced Penile Cancer Presenting With Renal Failureover 4 years ago
Questions Linger Around COVID-19’s Originover 4 years ago
The Future of Telehealth for Hematology/Oncology CareNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.