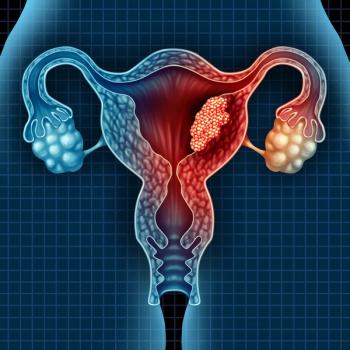
Early Chemo Does Not Improve Survival in Endometrial Cancer
Endometrial cancer survival correlates with total number of chemotherapy cycles – but not whether they are started earlier than radiation, according to the results of a new study.
The overall survival (OS) and cancer-specific survival (CSS) rates were not improved by receiving early chemo, defined as adjuvant chemotherapy before adjuvant radiation therapy, either with or without additional chemo “sandwich” regimens, according to the study in the American Journal of Clinical Oncology.
“No differences in OS or CSS were noted among endometrial patients receiving early chemotherapy,” concluded the authors, from the Huntsman Cancer Institute at the University of Utah. “However, the number of chemotherapy cycles was associated with prolonged survival.”
Patients that received both chemo and radiation for their endometrial cancer were selected from the SEER-Medicare database; 597 were selected. The median age was 72 years, and 85% of the patients were white.
Sixty-eight percent of the women had stage III disease, as defined by the International Federation of Gynecology and Obstetrics (meaning the cancer had spread into the pelvis, but not beyond). Some 77% of the patients received between 4 and 6 cycles of chemotherapy, with the remainder having either 1 to 3 cycles, or 7 or more.
Univariate and multivariate Cox proportional hazards regression was employed to understand the impact of clinical and demographic factors on the OS calculations, according to the authors.
For the group that received early chemotherapy, the 5-year survival marks were not statistically improved. The OS was 66.6% vs 62.4% for the early and standard of care groups, respectively (P = 0.46), and the CSS was 71.1% vs 71.2% (P = 0.88), the data showed.
The multivariate analyses determined the OS hazard ratio was 0.87 (95% CI: 0.56-1.34, P = 0.53), and the CSS HR as 1.21 (95% CI: 0.82-1.79, P = 0.34), according to the results.
But the 4-to-6-chemo group fared better in OS, with a HR of 0.48 (95% CI: 0.26-0.87; P = 0.02). Seven or more chemo cycles meant an even more improved OS effect (HR=0.42, 95% CI: 0.20-0.89, P = 0.02), the investigators added.
Chemotherapy is not typically used in stage I and II endometrial cancers, according to the American Cancer Society.
Some of the standard-of-care practices in treating endometrial cancer have been questioned by researchers recently. According to a study in The New England Journal of Medicine published in June, the combination of chemotherapy and radiation was not associated with longer relapse-free survival than chemo alone in stage III or IVA variants of the disease.
References:
Boothe D, Orton A, Kim J, et al. Does Early Chemotherapy Improve Survival in Advanced Endometrial Cancer? Am J Clin Oncol. 2019 Nov;42(11):813-817. doi: 10.1097/COC.0000000000000616.
Matei D, Filiaci V, Randall M, et al. Adjuvant Chemotherapy plus Radiation for Locally Advanced Endometrial Cancer. N Engl J Med. 2019 Jun 13;380(24):2317-2326. doi: 10.1056/NEJMoa1813181.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.