ESMO 2016: Slow-Growing Melanomas Are More Sensitive to Pembrolizumab, Nivolumab
Objective tumor responses to pembrolizumab (Keytruda) and nivolumab (Opdivo) are associated with longer times between melanoma diagnosis and treatment.
Objective tumor responses to pembrolizumab (Keytruda) and nivolumab (Opdivo) are associated with longer times between melanoma diagnosis and treatment, according to a single-institution study presented (abstract
“Melanomas with slow natural history exhibit a higher sensitivity to nivolumab and pembrolizumab,” reported Nora Kramkimel, MD, of the Department of Dermatology, Hospital Cochin, in Paris, France, and coauthors, in a research poster presentation.
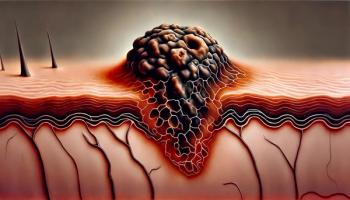
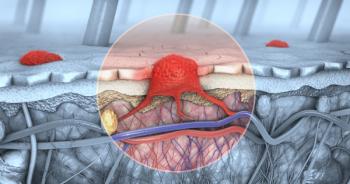
Programmed cell death protein 1 (PD-1) is an immune T-cell surface receptor that functions as an immune checkpoint that inhibits T-cell activation. It promotes immune tolerance of patients’ own cells, but can help tumors escape immune attack. Anti-PD-1 antibodies like nivolumab and pembrolizumab are used in immune checkpoint blockade immunotherapy, improving antitumor immune cell response.
PD-1 targeting immune checkpoint blockade offers excellent responses for some patients with advanced melanoma, but others’ tumors fail to respond; “little is known” about why that might be or predictive factors, the study authors noted. They therefore investigated melanoma natural history variables to identify predictive correlates of immunotherapy response.
The researchers retrospectively reviewed 65 patients’ cases of advanced melanoma (31 females, median age 65 years) diagnosed between August 2014 and January 2016, using RECIST 1.1 objective response criteria. Only patients who received more than one infusion were included in the study, and patients with “only in-transit” metastases (stage N2c tumors) were excluded. Twenty-eight percent of the tumors harbored BRAF V600 mutations, the team reported.
Treatment was initiated at disease progression; 73% were administered pembrolizumab and 27% received nivolumab. Anti-PD-1 therapy had been the first-line treatment for 36% of patients in the study.
Objective response rate was 40% and the mean time-in-node (the delay between first lymphatic metastasis and first visceral metastasis) was 26 months (range, 2 to 132 months).
“There was no statistical correlation between response and either lymphatic vs hematogenous dissemination or time-in-node,” they reported.
However, average time-to-treatment (delay between diagnosis and initiation of PD-1 therapy) was associated with objective response (a mean of 99 months among responders versus 53 months in nonresponders; P = .01).
“The same analysis with time from diagnosis to first-line therapy was also positive,” they noted (a mean of 85 months versus 45 months in responders and nonresponders, respectively; P = .02).
The coauthors reported no conflicts of interest.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.