Ipilimumab and Melanoma: Rejoicing, Disappointment, and Threat
The monoclonal antibody ipilimumab provides the first hopeful option ever for patients with metastatic melanoma. It has some peculiar qualities: Bad side effects are a good sign, and progression after treatment isn't necessarily a bad one.
Last week Greg Freiherr wrote in this space about the
There's also new life for monoclonal antibodies, which science journalists touted as the Next Miracle of Molecular Medicine, way back in the last century. Monoclonal antibodies were portrayed as special forces sent direct to the enemy, given special intelligence. (We're paying the price now for that kind of hype, in terms of patients turned cynical about mainstream health care.)
Today, decades later, there's a real story to tell about monoclonal antibodies and cancer. The special agents actually can kill the enemy, because our intelligence is much better now. But it was hard-won. This is
Announced concurrently in the
In a randomized study involving 125 cancer centers in 13 countries on 4 continents, 46% of metastatic melanoma patients given the antibody as monotherapy were alive after a year, and 24% survived for two years. (The disappointment part, of course, is for the 76% of patients who did not, and for their families and doctors.)
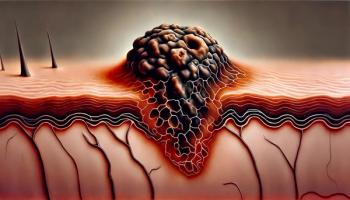
Ipilimumab targets CTLA-4 (cytotoxic T-lymphocyte associated antigen 4), which is the best-known of the "
CTLA-4 is part of the self-recognition process that normally restrains T lymphocytes from over-reacting in peripheral tissues after a challenge, which has the effect of inhibiting the lymphocytes' antitumor response. Ipilimumab counteracts this, and anti-cancer immunotherapy (in melanoma, at least) triumphs.
The NEJM study results, announced concurrently at ASCO, reveal the success of ipilimumab as monotherapy against metastatic melanoma. They also clarify that adjuvant treatment with antitumor vaccine gp100 (based on a protein from the melanoma cell surface) makes no difference.
Other reports at ASCO provide further detail.
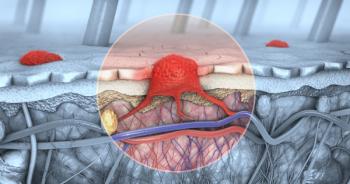
• Although ipilimumab itself does not cross the blood-brain barrier, the newly activated T cells do. The first study to test its effect against brain metastases, a
• When progression sets in again after an initial course of the antibody, reinduction of ipilimumab again controls the cancer for at least two-thirds of patients with inoperable Stage III or IV melanoma. (This information comes from a
• The antibody's longest track record against metastatic melanoma comes from the NCI, where
Messing with the normal immune system is bound to have consequences, and predictably the chief side effects of ipilimumab are immune response adverse effects or IRAEs. (Ironically, "irae" is Latin for "anger.") These are primarily diarrhea, rashes, and pruritis, and they usually resolve after a few weeks with steroid treatment.
Monoclonal antibody treatment also shows several peculiarities. Unlike standard chemotherapy, side effects are a good sign, because they correlate with a strong antitumor response. And progressive disease may not always be a sign of treatment failure: Instead of stalling or shrinking, lesions may actually grow or increase in number during the course of ultimately successful treatment with ipilimumab. This unpredictability has led immunotherapy researchers to develop and adopt a system of
So what's the aforementioned threat? The cost, of course. The news about ipilimumab and melanoma quickly hit the
What story will be told about all of this in 20 years? On one hand, we now have actual molecular magic bullets and high-tech, high-cost medical care. On the other, we have health reform, a fragile economy, a thinner ozone layer, skimpy clothing, tanning parlors, and young people who seem always to feel invulnerable.
Inbetween are sunscreen, hats, vigilance, restraint, and difficult questions.
Who wants to tell that story, let alone hear it?
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.