Oncology NEWS International
- Oncology NEWS International Vol 16 No 5
- Volume 16
- Issue 5
The 'New' Medicare: Passive Payer No More; PQRI Is First Step
CMS is shifting from being a passive bill payer to becoming an active purchaser of value-based care
BALTIMORE, Maryland"CMS is shifting from being a passive bill payer to becoming an active purchaser of value-based care," Terrence Kay said at the 33rd Annual Meeting of the Association of Community Cancer Centers (ACCC).
Mr. Kay, director of the Centers for Medicare & Medicaid Services (CMS) Hospital Ambulatory Policy Group, said that controlling spending and increasing quality and efficiency are essential to the sustainability of the Medicare program. "We must increase the value and quality of the care the program purchases," he said.
The 2007 Physician Quality Reporting Initiative (PQRI) is a first step toward linking Medicare health professionals' payments to quality, which is consistent with Medicare's ongoing transformation from passive payer to active purchaser of high-value healthcare. "This voluntary initiative will provide a financial incentive to physicians and other eligible professionals who successfully report quality information related to services provided under the Medicare Physician Fee Schedule," he said. The PQRI is mandated under the Tax Relief and Health Care Act of 2006. "Under this pay-for-reporting (P4R) program, oncologists reporting on specific quality measures will be eligible for a 1.5% bonus (subject to a cap) of total allowed physician charges for covered services from July 1 to December 31, 2007. The bonus will be paid in the summer of 2008," he said. Claims must be submitted by February 2008. "The 1.5% bonus will be paid for 'successful' reporting of quality measures. If the quality measure is reported 80% of the time, it is considered 'successful' reporting," Mr. Kay said.
Of the overall 74 quality measures covered under the PQRI, Mr. Kay said there are four for hematology, three for medical oncology, one for radiation oncology, and one for documentation of treatment plan before chemotherapy administration.
Mr. Kay stressed that both private practice and hospital-based physicians, including physicians who are hospital employees, can participate in the 2007 PQRI. Among the other healthcare professionals who can report on quality measures are nurse practitioners, clinical nurse specialists, physician assistants, clinical social workers, clinical psychol-ogists, registered dietitians, nutrition professionals, physical therapists, and occupational therapists. Mr. Kay noted that eligible professionals who choose to participate in the PQRI will gain experience in capturing and submitting data on the quality of care they provide. Participants will receive confidential feedback reports regarding their practices.
Eligible professionals do not need to register for PQRI, Mr. Kay said, but can participate by reporting the appropriate quality measures data on Medicare claims, using the specified quality-data G codes that are currently under development. CMS is working with the American Medical Association to develop the CPT category 2 codes that will match each quality measure under the PQRI. The agency will provide detailed specifications that will link CPT codes and ICD-9 codes with each quality measure. To stay updated on the PQRI, Mr. Kay urged attendees to check the program's website at
Articles in this issue
almost 19 years ago
Escalating Drug Costs Could Provoke Consumer Backlashalmost 19 years ago
Large Study Casts Doubt on Value of CADalmost 19 years ago
Cetuximab Does Not Increase Mucositis in H&N Canceralmost 19 years ago
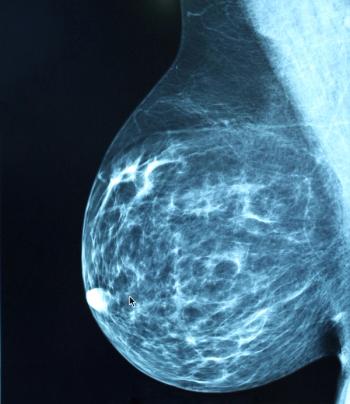
2004 Update Shows Continued Lower Breast Ca Incidencealmost 19 years ago
Reclast Single-Dose Infusion Approved for Paget's Diseasealmost 19 years ago
Fragmin Approved for VTE in Cancer Ptsalmost 19 years ago
New Phase III Trial of Genasense in Advanced Melanoma Plannedalmost 19 years ago
Cervical Cancer Vaccines Show Sustained Protectionalmost 19 years ago
ONI Reader Poll OnlineNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.