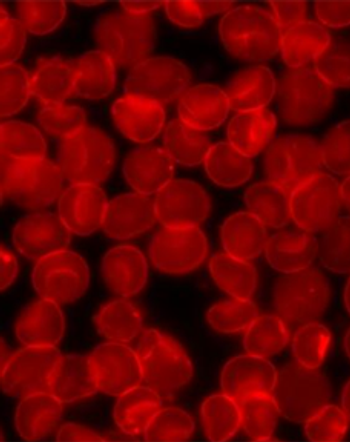
No Difference in Survival for Idarubicin, High-Dose Daunorubicin in AML
There was no significant survival difference in newly diagnosed acute myeloid leukemia patients given induction therapy with idarubicin vs high-dose daunorubicin.
There was no significant difference in treatment outcomes for patients with newly diagnosed acute myeloid leukemia (AML) given induction regimens with cytarabine plus idarubicin (AI) compared with cytarabine plus high-dose daunorubicin (AD), according to the results of a study
However, high-dose daunorubicin was more effective in patients with FLT3-ITD mutations.
“Although there were differences in patient characteristics regarding secondary leukemia and cytogenetic risk group between the two arms…multivariable and subgroup analysis showed that the imbalances did not have significant impact on the outcomes,” wrote researcher Je-Hwan Lee, MD, of the Asan Medical Center at the University of Ulsan College of Medicine in Seoul, Korea, and colleagues.
Recent studies have established high-dose daunorubicin as the standard of care for induction therapy in patients with AML; however, there were a lack of data showing if daunorubicin was superior to idarubicin in this patient population. Therefore, Lee and colleagues sought to compare these two regimens in young adults with newly diagnosed disease.
The study randomly assigned 299 patients to the AI arm (idarubicin 12 mg/m2 per day for 3 days; n = 149) or the AD arm (high-dose daunorubicin 90 mg/m2 per day for 3 days; n = 150).
Complete remission was achieved in 77.6% of patients in the study. There was no difference in the rate of complete remission in patients assigned to idarubicin compared with daunorubicin (80.5% vs 74.7%).
With a median follow-up of 34.9 months, survival was not significantly different for patients assigned idarubicin compared with high-dose daunorubicin. The 4-year overall survival rates were 51.1% compared with 54.7%, and the event-free survival rates were 45.5% compared with 50.8%, respectively.
The researchers did find an interaction between treatment with high-dose daunorubicin and the FLT3-ITD mutation. Among patients with the FLT3-ITD mutation, treatment with daunorubicin resulted in higher overall survival (P = .030) and event-free survival (P = .028). There were no significant differences in complete response or cumulative incidence of relapse.
“Our trial suggests that higher doses of daunorubicin are better than idarubicin in this population, although this finding should be confirmed in a larger randomized study,” the researchers concluded.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.