Patient Outcomes After Stopping Ruxolitinib Remains Dismal in Myelofibrosis
This study highlighted the need for novel therapies in myelofibrosis treatment, given that salvage therapies could potentially improve patient outcomes.
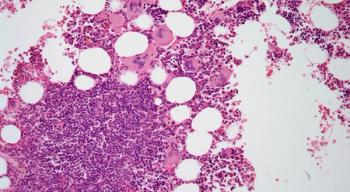
The outcome of patients with myelofibrosis (MF) after discontinuation of ruxolitinib (Jakafi) is poor, especially for those who discontinued in blast phase (BP), according to a study published in Cancer.
Researchers noted that salvage therapies could potentially improve patient outcomes, highlighting the need for novel therapies.
“Overall, we observed that outcomes were extremely poor for patients who had MF in BP regardless of treatment, whereas, for those in chronic phase, receiving a salvage therapy and particularly entering a clinical trial possibly may improve survival,” the authors wrote.
In this retrospective analysis, an electronic clinical database with data from 20 European hematology centers featuring clinical and laboratory data for 524 patients who received ruxolitinib after myelofibrosis was assessed. At 3 years, 40.8% of patients had stopped ruxolitinib. Baseline predictors of drug discontinuation were intermediate-2-risk/high-risk category (Dynamic International Prognostic Score System), a platelet count <100 x109 per liter, transfusion dependency, and unfavorable karyotype. At last contact, 51.1% patients had stopped therapy, and the median drug exposure was 17.5 months.
Fifty patients (18.7%) died while taking ruxolitinib. The reasons for discontinuation in the remaining 218 patients were the lack (22.9%) or loss (11.9%) of a spleen response, ruxolitinib-related adverse events (27.5%), progression to blast phase (23.4%), ruxolitinib-unrelated adverse events (9.2%), and allogeneic transplantation during response (5.1%). The median survival after ruxolitinib was 13.2 months and was significantly better in the 167 patients who discontinued ruxolitinib in chronic phase (27.5 vs 3.9 months for those who discontinued in blast phase; P < .001).
No survival differences were detected among patients who stopped ruxolitinib in chronic phase because of lack of response, loss of response, or ruxolitinib-related adverse events. The use of investigational agents and/or ruxolitinib rechallenge were correlated with improved outcome.
Failure to achieve or maintain a significant spleen response was the main cause of discontinuation, probably given that ruxolitinib is initiated in most patients to target this specific clinical need. However, researchers observed a counterintuitive decrease in baseline symptoms and splenomegaly at ruxolitinib discontinuation, indicating that ruxolitinib had some degree of efficacy, even in patients who eventually discontinued the drug.
Moreover, almost 20% of the patients stopped ruxolitinib due to the presentation of hematologic toxicity. This conclusion matched with the greater frequency of anemia and thrombocytopenia that the researchers detected at the time of ruxolitinib discontinuation.
Additionally, this study illustrated that infections might lead to discontinuation in a substantial fraction of ruxolitinib-treated patients, emphasizing the recommendation for close infectious monitoring before and during chemotherapy.
“This finding reflects the adherence of treating hematologists to prescribing information, according to which the ruxolitinib dose should be reduce in case of thrombocytopenia. Conversely, we observed that both anemia and thrombocytopenia comparably triggered reductions of the ruxolitinib dose,” the authors wrote. “This observation probably reflects that anemia is managed in real life with great caution and provides new insights into the practical management of ruxolitinib.”
This study did not provide the dynamics of non-driver mutations, which researchers noted are not recommended in a real-life context but were previously identified as very formative, however they did establish clinical and laboratory features that can conveniently be evaluated in everyday clinical practice and may be associated with the discontinuation of ruxolitinib and outcome.
According to the study, approximately 0.6 new cases of MF are established per 100,000 people per year.
Reference:
Palandri F, Breccia M, Bonifacio M, et al. Life After Ruxolitinib: Reasons for Discontinuation, Impact of Disease Phase, and Outcomes in 218 Patients With Myelofibrosis. Cancer. doi:10.1002/cncr.32664.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.