Oncology NEWS International
- Oncology NEWS International Vol 10 No 4
- Volume 10
- Issue 4
Procedure Reduces Blood Transfusion Need in Myelofibrosis
NEW YORK-Bone marrow ron-geur can free some patients with advanced myelofibrosis of the need for blood transfusions, Richard T. Silver, MD, clinical professor of medicine, Weill Medical College of Cornell University, said at the Chemotherapy Foundation Symposium XVIII. Dr. Silver’s major collaborators in the study were Dr. Malcolm Moore, a noted cell biologist at Memorial Sloan-Kettering Cancer Center, and Dr. Edward Athanasian, an orthopedic surgeon at the Hospital for Special Surgery, New York.
NEW YORKBone marrow ron-geur can free some patients with advanced myelofibrosis of the need for blood transfusions, Richard T. Silver, MD, clinical professor of medicine, Weill Medical College of Cornell University, said at the Chemotherapy Foundation Symposium XVIII. Dr. Silver’s major collaborators in the study were Dr. Malcolm Moore, a noted cell biologist at Memorial Sloan-Kettering Cancer Center, and Dr. Edward Athanasian, an orthopedic surgeon at the Hospital for Special Surgery, New York.
Dr. Silver and his colleagues used the rongeur procedure in 9 patients with myelofibrosis who required blood transfusions of 2 to 4 units per month and/or had massive splenomegaly. Seven patients required transfusions twice monthly, and two were admitted to the study because of increasing spleen size. Six patients, Dr. Silver noted, had splenectomy before or immediately after the rongeur procedure. The median age of the seven men and two women in the study was 65 years.
One patient died in the immediate postoperative period due to aspiration. Of the remaining eight patients, five responded to the treatment, Dr. Silver reported.
Two of the responders have died of causes other than myelofibrosis. One patient, Dr. Silver said, "was transfusion free with a hematocrit of 36 and a hemoglobin of 12 for a period of 3 years, when this individual died of a myocardial infarction at age 74." The other required no transfusions for 18 months before dying of pneumonia.
"Currently, 3 of the 9 patients are alive, leading perfectly normal lives, transfusion free," Dr. Silver said. "Although the hematocrits are not back to normal, they are in a range where their performance status is 0 to 1."
Arrows indicate sites of marrow reaming in the femur and iliac crest.
In the procedure, bone marrow is reamed from the femur and iliac crest (see Figure 1), and then previously collected stem cells are infused into the medullary cavity. The bone marrow curettage is performed, Dr. Silver explained, "to provide a favorable, compatible milieu" for the infused cells.
The treatment begins with G-CSF (Neupogen) stimulation for 7 to 10 days, Dr. Silver said. Stem cells are harvested during serial biopsies of the iliac crest, and CD-34 cells are isolated and cryo-preserved.
At surgery, retrograde reaming using an instrument approximately 25 mm long and 9 mm wide removes 16 to 20 cc of fibrous tissue, Dr. Silver said. After the cavity is filled with CD-34 cells, the femoral entry is plugged. The residual CD-34 cells are infused via a central venous catheter 14 days later.
Patients have been examined at 4- to 6-month intervals. As a result of these examinations and histologic studies, Dr. Silver said, "we have demonstrated that, in fact, these patients have documented morphologic evidence of recurrent hematopoiesis at the site of rongeur."
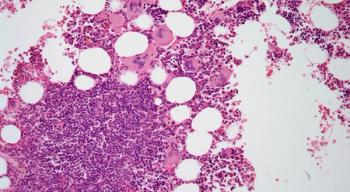
The autopsy of one of the patients who died, Dr. Silver noted, unequivocally showed recurrent hematopoiesis in the rongeured marrow (see Figure 2). The nonrongeured femur, he added, had persistent fibrosis.
Figure 2. In the image on the left, myelofibrosis and osteosclerosis are visible in the left femur prior to reaming. The image at right shows normal hematopoiesis in reamed marrow. Special stains (glycophorin and alkaline phosphatase stains) demonstrated early erythroid and myeloid elements.
As a result of the experience to date, Dr. Silver and his colleagues are evaluating the need to use G-CSF or erythropoietin (Epogen, Procrit) to stimulate progenitor cells, based on the studies of Dr. Moore.
Only postsplenectomy patients will have the rongeur treatment in the future, Dr. Silver added, "because we believe the chemokine gradient favors the stem cells going to the spleen rather than the femur."
The surgical procedure, he indicated, will be modified so that only the femur is reamed because the iliac crest did not add substantial hematopoietic sites.
The approach, Dr. Silver concluded, appears to benefit patients by altering the marrow microenvironment. "We believe that a functional hematopoiesis may be restored to support life without transfusions," he said. "We know it is not a cure because the natural history of the disease may be altered but not qualitatively changed."
Articles in this issue
almost 25 years ago
IOM Urges Action to Fix ‘Broken’ US Health Care Systemalmost 25 years ago
Thompson Pledges Fundamental HCFA Reformalmost 25 years ago
NCCN Updates Its Practice Guideline for Breast Canceralmost 25 years ago
Smoking Prevalence, Mortality Ranges Widely From State to Statealmost 25 years ago
NCI Debuts New Program for Cancer Advocatesalmost 25 years ago
Fiberoptic Ductoscopy for Nipple Discharge DisWomen With Nipple Dischargealmost 25 years ago
Augmerosen, Antisense Drug, in Phase III Testing in Melanomaalmost 25 years ago
Automated System Improves Accuracy of HER-2 Scoringalmost 25 years ago
Small Advantage for Adjuvant Paclitaxel in Early Breast CancerNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.