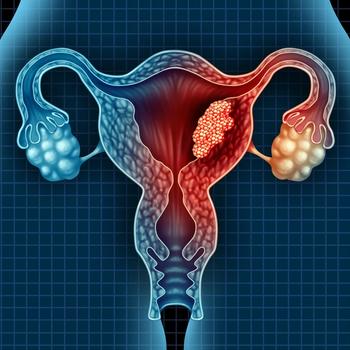
Study Identifies Factors of Microbiome Composition in Endometrial Cancer
A research team from the Mayo clinic verified the known risk factors for endometrial cancer, while identifying a possible microbiome signature associated with the disease.
Researchers from the Mayo Clinic have identified a microbiome signature associated with endometrial cancer, according to a study published in Scientific Reports.1
The signature is in part driven by postmenopausal status, along with additional known risk factors for endometrial cancer such as obesity and high vaginal pH (>4.5), which together significantly modify the composition of the reproductive tract biome and leads to an increased diversity. Previous studies have demonstrated that healthy vaginal microbiota is most commonly low in diversity and dominated by Lactobacilli species.
“Of the 17 taxa we found enriched in (endometrial cancer) patients, 8 were also enriched by postmenopause,” said the researchers. “Because postmenopausal status is a main risk factor for endometrial cancer, this system can be thought of as an ecological succession towards a disease state.”
The researchers collected microbiome samples from 148 women undergoing a hysterectomy for either endometrial cancer (n = 66) or other benign uterine conditions (n = 75). The samples were analyzed for diversity across multiple parameters identified as known risks for endometrial cancer. In the lower reproductive tract, both α- and β-diversity were associated with patient menopause status (P = 0.002 and P = 0.007, respectively). In the uterus, the microbiome α-diversity reached significance (P = 0.024), while β-diversity did not (P = 0.221).
“All parameters analyzed (menopause status, BMI, and vaginal pH) showed a significant impact on the microbiome composition, with postmenopause, obesity, and high vaginal pH significantly increasing the microbiome diversity,” noted the researchers. “Of note was the marked enrichment of Anaerococcus, Peptoniphilus, and Porphyromonas species.”
The analysis identified P. somerae as the microbe with the strongest association with endometrial cancer (P < 0.001), which was present in all patients with type II disease and in 57% of those with hyperplasia.
“We know other cancers (cervical, gastric cancers) are associated with certain infections (HPV and H. Pylori, respectively,) so it is intriguing to think that there may be micro-organisms associated with the development of other cancers such as endometrial cancer,” commented Elizabeth Etkin-Kramer, MD, FACOG, assistant professor of gynecology at Florida International University, Herbert Wertheim School of Medicine, who was not involved in the study.
In addition to the small sample size and lack of diversification of those samples, a noted limitation of the study was the poor overall health of the patients without endometrial cancer.
“These hysterectomy patients came to Mayo Clinic due to abnormal bleeding, pain, or some combination of these,” wrote the researchers. “These were not healthy women.”
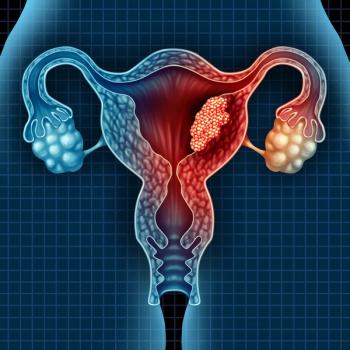
Still, the suggested association of a specific microbiome signature for endometrial cancer is enough to warrant further research – with the long-term goal of possibly developing a screening test for the disease.
“If the micriobiome does play a role in endometrial cancer, beyond being a marker for it, this could have important implications for endometrial cancer prevention,” said Maria Walther-Antonio, PhD, of the Miocrobiome Program, Center for Individualized Medicine, Mayo Clinic, Rochester, MN, in a press release.2
“We need larger studies to further confirm an association of certain microorganisms in women with endometrial cancer compared to our healthy women in our office. If so, perhaps a non-invasive screening test confirming the presence of this organism in the vaginal microflora would allow for subsequent evaluation of these women for earlier detection of endometrial cancer,” said Etkin-Kramer, before adding “anything that will help prevent a cancer or detect a cancer at its earliest, most treatable stage is definitely a plus.”
Reference:
1. Walsh DM, Hokenstad AN, Chen J, et al. Postmenopause as a key factor in the composition of the Endometrial Cancer Microbiome (ECbiome).
2. Mayo Clinic researchers look at post menopause as key factor in endometrial cancer [news release]. Mayo Clinic. Rochester, Minnesota. Published December 16.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.