Symptom Burden of Polycythemia Vera Substantial
A new study has confirmed that the symptom burden of patients with polycythemia vera is substantial, and is independent of a patient’s disease features.
A
“The results of this investigation plainly show that symptoms in patients with PV who have known hydroxyurea use, known phlebotomy requirements, and splenomegaly are greater than in those patients who lack these features,” wrote Ruben A. Mesa, MD, of the Mayo Clinic in Scottsdale, Arizona, and colleagues in the Journal of Clinical Oncology. “Furthermore, there is an additive effect on symptom burden as more features are included in a patient’s profile.”
According to background information in the study, a large number of patient with PV have undermanaged symptom burden despite being treated for the condition. These symptoms can include fatigue, pruritus, night sweats, fever, and more.
In 2014, ruxolitinib was approved for patients with PV who are resistant or intolerant to hydroxyurea, a first-line treatment for patients with PV who need cytoreductive therapy. However, according to Mesa and colleagues, “this tremendous advancement for the PV population is limited by the issue of the restricted availability of ruxolitinib to select PV patients whose baseline symptomatology has not yet been fully characterized or compared to other PV patients who lack hydroxyurea resistance/intolerance but still potentially face high symptom burdens.”
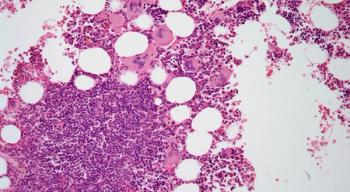
Therefore, Mesa and colleagues prospectively evaluated 1,334 patients with PV with characterized symptom burden. Using the MPN-SAF Total Symptom Score (TSS), they assessed fatigue, early satiety, abdominal discomfort, inactivity, concentration problems, night sweats, itching, bone pain, fevers, and weight loss. The researchers also assessed patient demographics, laboratory data, and the presence of splenomegaly by disease feature (known hydroxyurea use [PV-HU, n = 499], known phlebotomy requirements [PV-P, n = 646], palpable splenomegaly [PV-S, n = 369], or all three [PV-HUPS, n = 148]).
Results indicated that the presence of each disease feature by itself was associated with a moderately high symptom burden that persisted despite a patient’s PV risk category. The MPN-SAF TSS was 29.2 for PV-HU, 27.7 for PV-P, and 28.8 for PV-S.
The researchers found that the symptoms incrementally increased in severity with the addition of other disease features. As such, those patients with PV-HUPS had the highest total symptom score of 32.5.
“With the 2013 symptom response thresholds criteria, patients with PV who had all three features (PV-HUPS) met criteria for symptom quartile 4 (TSS, 32.5; high symptom burden profile),” the researchers wrote. “To put this into perspective, the average TSS of patients with myelofibrosis falls within symptom quartile 3 (TSS, 25.3), which suggests that disease burden is exceptionally high within this PV population.”
However, the researchers also noted that patients with only one disease feature also ranked within symptom quartile 3, demonstrating a suboptimal symptom control.
“The symptom burdens of patients with PV who have splenomegaly and/or phlebotomy requirements remain unacceptably high and rival those of patients who meet high-risk criteria and who, therefore, become candidates for hydroxyurea treatment,” they wrote. “These findings are far-reaching because emerging therapies offer the potential to reduce phlebotomy requirements, protect against vascular events, improve the symptomatic burden, and potentially offer protection against disease transformation.”
Based on the results of this study, Mesa and colleagues suggested that patients with PV who have one or two disease features may benefit from JAK2 inhibitor treatment.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.