Articles by Eduardo Bruera, MD
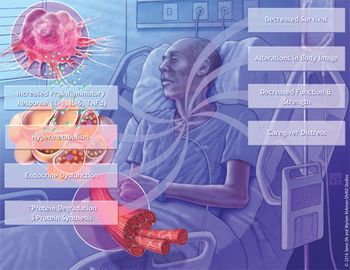
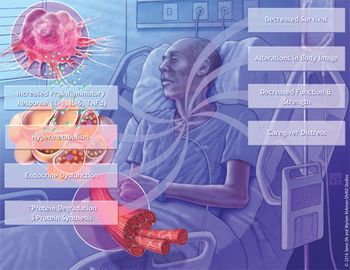
Cancer patients are often referred for cachexia intervention treatments late in their disease trajectory-that is, at a point where attempts to reverse the weight loss process may be less beneficial. In addition, healthcare professionals frequently under-recognize the prevalence of cancer cachexia, and this may contribute to delayed treatment of weight loss, often until the refractory stage.

Fatigue and dyspnea are two of the most common symptoms associated with advanced cancer. Fatigue is also commonly associated with cancer treatment and occurs in up to 90% of patients undergoing chemotherapy.

Pain in older cancer patients is a common event, and many times it is undertreated. Barriers to cancer pain management in the elderly include concerns about the use of medications, the atypical manifestations of pain in the elderly, and side effects related to opioid and other analgesic drugs. The care of older cancer patients experiencing pain involves a comprehensive assessment, which includes evaluation for conditions that may exacerbate or be exacerbated by pain, affecting its expression, such as emotional and spiritual distress, disability, and comorbid conditions. It is important to use appropriate tools to evaluate pain and other symptoms that can be related to it. Pain in older cancer patients should be managed in an interdisciplinary environment using pharmacologic and nonpharmacologic interventions whose main goals are decreasing suffering and improving quality of life. In this two-part article, the authors present a review of the management of pain in older cancer patients, emphasizing the roles of adequate assessment and a multidisciplinary team approach.

Pain in older cancer patients is a common event, and many times it is undertreated. Barriers to cancer pain management in the elderly include concerns about the use of medications, the atypical manifestations of pain in the elderly, and side effects related to opioid and other analgesic drugs. The care of older cancer patients experiencing pain involves a comprehensive assessment, which includes evaluation for conditions that may exacerbate or be exacerbated by pain, affecting its expression, such as emotional and spiritual distress, disability, and comorbid conditions. It is important to use appropriate tools to evaluate pain and other symptoms that can be related to it. Pain in older cancer patients should be managed in an interdisciplinary environment using pharmacologic and nonpharmacologic interventions whose main goals are decreasing suffering and improving quality of life. In this two-part article, the authors present a review of the management of pain in older cancer patients, emphasizing the roles of adequate assessment and a multidisciplinary team approach.

Cancer causes pain as it invades bone, compresses nerves, produces obstructive symptoms in the pulmonary, gastrointestinal, and genitourinary systems, and distends involved visceral organs. This manuscript reviews progress in cancer pain management during the past 2 decades. Since the 1980s, we have seen (1) genuine advances in research on the biology of pain, (2) new approaches to the treatment of cancer pain, and (3) important changes in the health-care system to ensure that pain is appropriately assessed and managed. Currently, clinicians have the appropriate diagnostic and therapeutic tools to ensure that the vast majority of patients with cancer pain can be comfortable during their illness. Nevertheless, too many patients with terminal malignancies continue to die in pain in nations around the globe. An effective strategy to make alleviating pain a major health-care priority remains the primary challenge to effectively palliating patients with cancer pain.

The authors of abstract #2396 conducted a 6-week trial of thalidomide (Thalomid), 100 and 200 mg at bedtime, in 15 cachectic patients. The main findings of this uncontrolled study were cessation of weight loss, increased body fat percentage,

Drs. Choi and Billings provide an excellent summary of the historical developments, clinical issues, and ethical dilemmas associated with palliative care. As they recount, the British hospice movement of the 1960s began as a fringe movement away from the main academic centers and organized medicine. This separation provided a safe environment in which palliative-care practitioners could deliver clinical care while establishing a new body of knowledge. On the other hand, because of this lack of connection, palliative care is still not recognized as a specialized area of medical practice in many countries, including the United States. This perception persists despite the fact that palliative care developed earlier than other fully recognized subspecialties such as emergency medicine and critical care.

The optimal management of opioid-related side effects is hampered by a lack of comparative studies of management strategies. The prevalence of such side effects is influenced by the extent of disease, the patient’s

This article on the management of breakthrough pain by Simmonds is one of a number of excellent reviews on the palliative aspects of cancer care published in ONCOLOGY over the last 2 years. Breakthrough pain is a frequent, poorly understood

Passik and colleagues address an important and badly neglected issue in cancer care. Alcoholism has been reported to occur in 5% to 15% of the North American population, and drug abuse in approximately 5%. In hospitalized patients, the prevalence of alcoholism increases to approximately 20%.[1] In 200 patients admitted to a tertiary palliative care program in a health care system providing universal access, the prevalence of alcoholism was 27%.[2]

Patient-controlled analgesia (PCA) is a relatively new technique in which patients are able to self-administer small doses of opioid analgesics when needed. Many different devices are available for opioid infusion, including