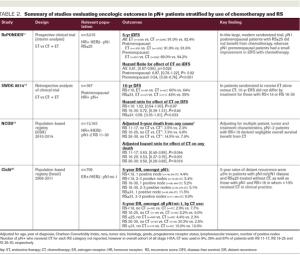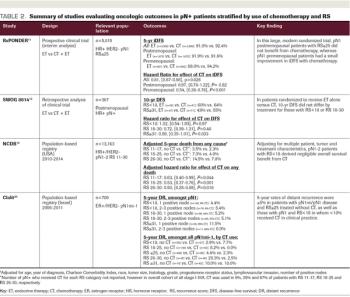
ABSTRACT The 21-gene Recurrence Score (RS) assay has been validated as both a prognostic and predictive tool in node-negative (pN0), estrogen receptor–positive (ER+), HER2-negative (HER2–) breast cancer. A large body of evidence supports the clinical utility of the RS in the node positive (pN+) population as well. Retrospective analyses of archived tissue from multiple clinical trials have found the RS to be prognostic in both endocrine therapy (ET)-treated and chemotherapy-treated patients with pN+ disease. Distribution of RS results in pN+ patients have also been consistent with those of pN0 populations. Data from the SWOG 8814 trial and large population-based registries further support the prognostic and potential predictive value of the RS. Specifically, patients with 1 to 3 positive nodes and RS less than 18 derived negligible benefit from adjuvant chemotherapy in these studies. In the prospective West German Study Group PlanB and ADAPT trials, pN+ patients with RS less than 11 and RS ≤25, respectively, who were treated with ET alone experienced excellent outcomes. Finally, 5-year results of the RxPONDER clinical trial randomizing patients with 1 to 3 positive nodes and RS ≤25 to ET alone vs ET plus chemotherapy confirmed an absence of chemotherapy benefit in postmenopausal patients. Clinical practice guidelines support use of the RS in the pN+, ER+/HER2– population, and many institutions have adopted the RS to guide clinical decision-making, resulting in a net reduction of adjuvant chemotherapy use. This review highlights the existing data supporting the prognostic and predictive ability of the RS in pN+ disease, current practice patterns related to RS use in this population, and emerging applications.