
“Promising” Data Support Blinatumomab in CD19+ B-ALL Population
Overall survival data with blinatumomab in the phase 3 E1910 study may be an “important development” in CD19-positive B-ALL.
“Incredibly promising data” from the phase 3 E1910 trial (NCT02003222) appear to support the use of blinatumomab (Blincyto) as a treatment for patients with CD19-positive Philadelphia chromosome–negative B-cell precursor acute lymphoblastic leukemia, according to Colin A. Vale, MD.
In a conversation with CancerNetwork® ahead of the
Specifically, Vale highlighted a significant overall survival (OS) improvement with blinatumomab following chemotherapy compared with chemotherapy alone in the trial. This OS improvement may represent an “important development” given the high incidence of relapse following induction chemotherapy.
According to findings presented at the
Transcript:
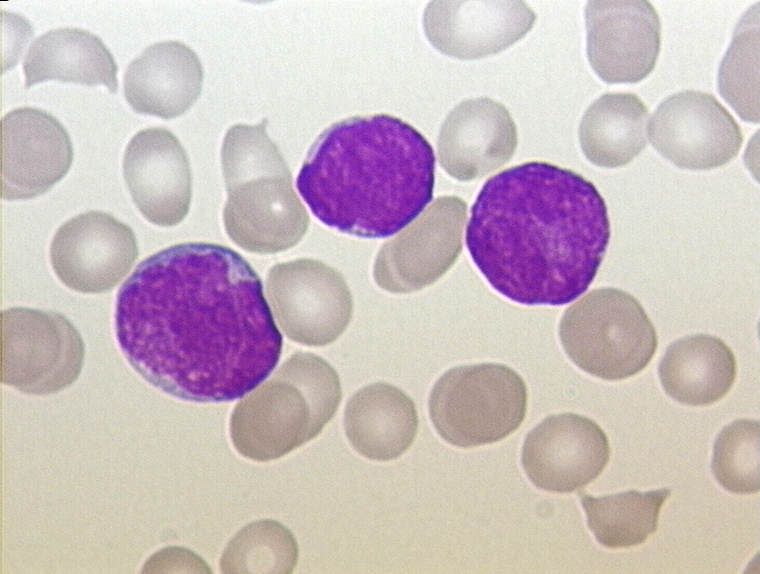
This is an exciting development. The bispecific T-cell engager blinatumomab, which targets the surface antigen CD19, has already received FDA approval in the relapsed/refractory and MRD-positive settings. The FDA is now reviewing the application in early-stage disease based on some incredibly promising data from the E1910 phase 3 randomized clinical trial. In this trial, patients with newly diagnosed Philadelphia chromosome—negative B-ALL were [randomly assigned] to receive either blinatumomab plus chemotherapy or chemotherapy [alone] following remission, induction, and intensification courses prior to receiving maintenance.
At a median follow-up of approximately 3 and a half years, overall survival was statistically significantly better in the patients who received blinatumomab. This is a critically important development, as ALL is the second most common cause of acute leukemia in adults. Despite high initial rates of remission following induction chemotherapy, relapses are unfortunately common [following] our standard consolidation and maintenance approaches. This represents an unmet need in terms of further reducing relapse risk in this patient population.
References
- FDA approved blinatumomab as consolidation for CD19-positive Philadelphia chromosome-negative B-cell precursor acute lymphoblastic leukemia. News release. FDA. June 14, 2024. Accessed June 14, 2024. https://shorturl.at/o5BTQ
- Litzow M, Sun Z, Mattison R, et al. S115: Consolidation with blinatumomab improves overall and relapse-free survival in patients with newly diagnosed B-cell acute lymphoblastic leukemia: impact of age and MRD level in ECOG-ACRIN E1910. Hemasphere. 2023;7(suppl ):e1944062.doi:10.1097/01.HS9.0000967372.19440.62
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.



































