Are Pap Smears Still Necessary?
It’s that time again: time for resolutions, a new start, and scheduling those dreadful annual health exams.
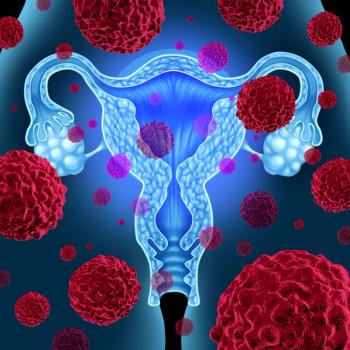
Thanks to the Pap smear, we are not only able to detect cervical cancer, but also premalignant cervical changes responsible for cervical malignancies.
HPV has been widely understood to be the most common
So what’s the link between HPV and cervical cancer?
Persistent infection with high-risk HPV types -- especially types 16 and 18 -- are responsible for approximately 70% of cervical cancer cases worldwide.
Cervical cancer screening used to be quite a simple concept for the lay person: "I go to my Gyn for my annual exam, and I automatically get a Pap smear," But times have
This brings us to the new debate: HPV-only testing.
Last year, the FDA announced the
The approved HPV test could be considered a primary cervical cancer screening tool in women aged 25 and over.
There are generally two sides to an argument. Dr. Warner Huh of the University of Alabama stated, "Pap smears are probably missing a fair amount of pre-cancer and cancer in women… The HPV test really outperforms Pap smears when it comes to cancer detection as well as precancerous detection."
Dr. Diana Zuckerman of the National Center for Health Research argues that with so many women contracting HPV without progression to cancer, this method could cause women to undergo unnecessary testing. Additionally, while HPV causes most cervical cancer cases, it does not cause all, and Dr. Zuckerman expresses a valid concern about that: “You could definitely miss out on some women who will in fact develop cervical cancer."
What are your thoughts on this debate? Should the HPV test replace the Pap smear or supplement it?
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.