Blood Screening for Early-Stage Lung Cancer Possible
A simple blood draw to evaluate cfDNA might one day be used for early-stage lung cancer screening-if the mutational “noise” of normal aging can be addressed.
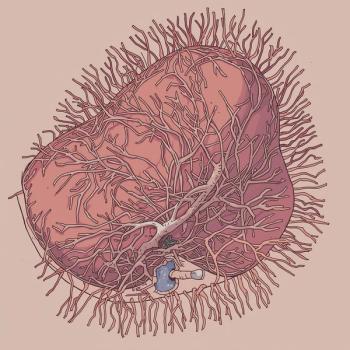
It is possible to detect early-stage lung cancer by sequencing circulating cell-free tumor DNA (cfDNA), suggest preliminary findings from the Circulating Cell-Free Genome Atlas (CCGA) study (
The initial results show that early-stage lung cancer can be detecting using genome sequencing of blood samples, reported lead study author Geoffrey R. Oxnard, MD, of Dana Farber Cancer Institute and Harvard Medical School in Boston.
“These are promising early results, and next steps are to further optimize the assays and validate results in a larger group of people,” Oxnard said. “Assays detected lung cancer across stages, histologies, and populations.”
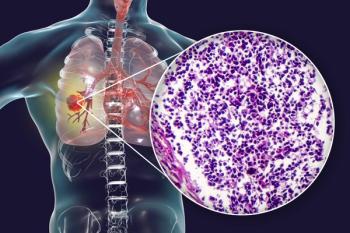
So-called “liquid biopsies” are already in use for patients with advanced lung cancer, to help identify targeted therapy options.
But lung cancer survival rates are significantly improved with early diagnosis.
Low-dose computed tomography (LDCT) is the current gold standard for lung cancer screening, but few high-risk people undergo LDCT exams, in part because of a relatively high rate of false-positive results which can prompt unnecessary invasive procedures. Genomic testing of plasma cfDNA might prove to be a simpler screening test for lung cancer and could detect targetable tumor gene signatures, Oxnard noted. “There is an unmet need globally for early detection tests for lung cancer that can be easily implemented by healthcare systems,” he said.
To date, the CCGA study authors have enrolled 12,292 of 15,000 intended participants, Oxnard reported. Seventy percent of the enrolled participants have cancer diagnoses.
Their preplanned preliminary analysis of 2,800 patient plasma samples were used for a “training” set from 1,733 patients with clinically evaluable cancers-127 of whom have lung cancers. And a second “test” set of 980 clinically evaluable patients’ samples (including 47 lung cancers) were also included in the analysis. Findings for the 127 patients with stage I–IV lung cancer were reported.
Three genomic assays were used to detect lung cancer cfDNA: targeted sequencing of somatic mutations, including single nucleotide polymorphisms, or SNPs, and INDEL mutations; whole-genome sequencing to detect tumor-gene copy number aberrations; and whole-genome bisulfite sequencing (WGBS) of cfDNA to detect epigenetic abnormalities.
Comparable “signals” of lung cancer were detected using all three assays and were more pronounced with more advanced stages of lung cancer, Oxnard reported. The findings show that cfDNA sequencing holds promise as a lung cancer screening tool with low false-positive rates.
WGBS testing detected 41% of stage I, II, and IIIA lung tumors, and 89% of late-stage (IIIB–IV) lung cancers. Whole-genome sequencing detected 38% of early-stage lung cancers and 87% of late-stage cases. Targeted sequencing detected 51% of early-stage and 89% of late-stage lung tumors.
False-positive findings were rare. Fewer than 1% of noncancer patient samples yielded a consistent “cancer-like” signal, Oxnard reported. Much more research is needed before the tests are ready for clinical use, however.
More than half (54%) of somatic mutations detected were from patient leukocytes rather than DNA shed into the bloodstream by lung tumors. Such mutational “noise” accumulates as a natural part of the aging process and must be reliably differentiated from tumor cfDNA, Oxnard cautioned. “White blood cell–derived mutations and copy number variations are a significant source of potential false-positives that must be accounted for to obtain high specificity,” he explained.
“We’re one step closer to being able to detect early lung cancer from a simple blood test,” commented ASCO Expert David Graham, MD, of the Levine Cancer Institute, Charlotte, North Carolina.
The study was funded by GRAIL, Inc.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.