- ONCOLOGY Vol 11 No 9
- Volume 11
- Issue 9
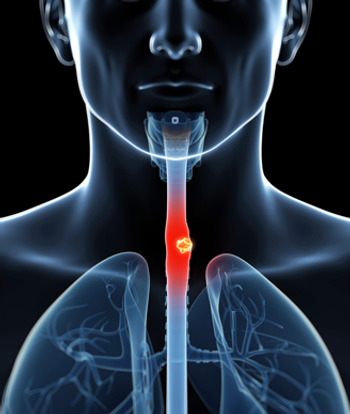
Combined-Modality Treatment of Esophageal Cancer
The use of chemotherapy and radiotherapy prior to surgery for patients with potentially resectable esophageal carcinoma has been investigated since the late 1970s, with trials yielding response rates approaching 50%.
ABSTRACT: The use of chemotherapy and radiotherapy prior to surgery for patients with potentially resectable esophageal carcinoma has been investigated since the late 1970s, with trials yielding response rates approaching 50%. Although some of these trials suggested improved survival with preoperative chemoradiation plus surgery, as compared with historical controls treated with surgery or radiation alone, the question of survival benefit had to be addressed in prospective, randomized fashion. This review describes the experience with surgery or radiation alone vs preoperative chemoradiation in terms of long-term overall survival in the treatment of esophageal cancer. [ONCOLOGY 11(Suppl 9):63-67, 1997]
Esophageal carcinoma is relatively rare in the United States, accounting for about 1% of cancers diagnosed each year. However, there are markedly different patterns of prevalence in other parts of the world.[1] High-incidence areas include India, southern Africa, northern Iran, and northern China.
Until recently, squamous-cell carcinoma comprised the vast majority of cases of esophageal cancer. However, the incidence of adenocarcinoma in white males has been rapidly increasing by approximately 10% per year for the past 10 years. This percentage increase in frequency exceeds that of all other cancers for that time period.[2,3] The prognosis for patients with either type of tumor histology appears to be poor.
The two predominant risk factors for the development of esophageal squamous-cell carcinoma are alcohol and tobacco abuse.[4] Adenocarcinoma has been linked to Barrett's metaplasia of the esophageal mucosa as a consequence of chronic gastroesophageal reflux disease. The prevalence of adenocarcinoma in association with Barrett's metaplasia has been found to range from 3% to 16% in various reported series.[5-7]
Esophageal cancer patients who have clinically metastatic disease at the time of diagnosis have a median survival of 6 months. Even patients with potentially localized, resectable disease who are treated with surgery have a median survival of approximately 12 months and a 5-year survival of 11% to 14%.[1]
The poor prognosis of esophageal cancer relates to its tendency for early spread into the submucosal lymphatic network, as well as to the absence of the serosal layer of the esophagus, which potentially limits local disease extension. Microscopic and/or gross disease is often present in lymph node or distant metastatic sites by the time the primary tumor becomes large enough to cause symptoms of dysphagia. Because of the frequency of disease dissemination at presentation, recent investigations have used systemic therapy combined with locoregional therapies to gain better local control and manage the systemic component of esophageal malignancy.
The potential benefits from adding preoperative chemotherapy include downstaging the disease to facilitate surgical resection, preventing local recurrence, and eradicating micrometastatic disease. At the time of surgery, response to chemotherapy can be assessed directly. The disadvantages of preoperative chemotherapy include the potential emergence of drug-resistant clones and the delay in definitive treatment with the risk of disease progression.
Randomized Trials
Four randomized trials have compared preoperative chemotherapy to surgery alone.
- Roth et al[8]reported a small study from The M.D. Anderson Cancer Center in which 39 patients were randomized to treatment with either surgery alone or preoperative chemotherapy with cisplatin (Platinol), vindesine, and bleomycin (Blenoxane), followed by surgery and postoperative chemotherapy with cisplatin and vindesine for 6 months. Despite a good chemotherapy response of 47%, the two arms had identical median survival rates of 9 months.
- SchlagIn a second randomized study, reported by Schlag,[9] 46 patients were randomized to either surgery or three cycles of preoperative chemotherapy with cisplatin and fluorouracil (5-FU) followed by surgery. At a median follow-up of 20 months, an interim analysis was done. Resectability rates were similar: 79% for the chemotherapy/surgery group and 77% for the surgery group. Median survival was 10 months for each group. The study was stopped, and the authors concluded that preoperative chemotherapy did not increase surgical resectability or survival for patients with esophageal carcinoma.
- Norwegian StudyA study by Nygaard et al[10] from Norway randomized 187 patients to one of four treatments: surgery alone, preoperative chemotherapy and surgery, preoperative radiation and surgery, or preoperative chemotherapy followed by radiation and then surgery. There was no significant difference in survival rates between the preoperative chemotherapy group and the surgery alone group (3-year survival rates of 3% and 9%, respectively).
- Intergroup TrialThe United States Intergroup completed a two-arm randomized trial, which compared three cycles of preoperative cisplatin/5-FU followed by surgery and postoperative cisplatin/5-FU vs treatment with surgery alone. Over 400 patients were enrolled. Until the mature results of this trial are known, use of preoperative chemotherapy must be considered investigational, since all completely reported randomized trials have been negative.
Patterns of relapse for esophageal carcinoma include both locoregional recurrence and distant metastases. Therefore, the combination of radiation and chemotherapy before surgery has been used in an attempt to improve both local and distant control.
Nonrandomized Studies
Several studies have used preoperative cisplatin and 5-FU plus radiation:
RTOG/SWOG StudiesTwo studies independently conducted by the Radiation Therapy Oncology Group (RTOG)[11] and the Southwest Oncology Group (SWOG)[12] tested a nearly identical treatment regimen of cisplatin and 5-FU combined with 30 Gy of radiation. Operability was 66% and 63%, respectively. Potentially curative resection was not reported in the RTOG study and was only considered to be 49% in the SWOG study.
Median survival in the RTOG study was 13 months, and 2- and 3-year survival rates were 15%, and 8%, respectively. In the SWOG study, median survival was 14 months, and 2- and 3-yer survival rates were 28%, and 16%. In both studies, patients who achieved a histologic complete response (CR) to the preoperative treatment regimen (27% in the RTOG study and 25% in the SWOG study) had improved overall survival after surgical resection.
St. Louis University StudyNaunheim et al[13] reported a study from the St. Louis University Medical Center in which 47 patients (29 squamous-cell carcinoma and 18 adenocarcinoma) were treated with simultaneous cisplatin, 5-FU, and 3,000 to 3,600 cGy of radiation preoperatively. Thirty-nine of these patients went to surgical exploration, and 83% (72% of the total group) were resectable. Overall median survival was 23 months, and 3-year actuarial survival was 40%. These survival results were significantly better than those of a group of historical controls from the same institution treated with either surgical resection or radiation, who had a median survival of 10.5 months and 0% with a 3-year survival.
University of Michigan StudyOne of the most promising results with combined preoperative chemoradiotherapy came from a trial conducted at the University of Michigan Medical Center. Forastiere et al[14] treated 43 patients with an intensive 21-day in-patient regimen of chemoradiation followed by surgical resection. Fluorouracil (5-FU) was administered as a continuous infusion for 21 days, and cisplatin and vinblastine (Velban) were given on days 1 to 5 and 17 to 21. Radiation was delivered concomitantly to a total dose of 3,750 to 4,500 cGy, followed by surgical resection 3 to 4 weeks later. Of the 43 patients, 22 had squamous-cell carcinoma and 21 had adenocarcinoma. The vast majority (95%) of patients completed the preoperative treatment even though toxicity was substantial, and 84% had a potentially curative resection. In 24% of the patients, no residual tumor was found in the resected esophagus.
The final report of this study was recently published, with a median follow-up of 78.7 months.[15] The median survival for all patients was 29 months, which was a major improvement from the 12-month median survival of a group of historical control patients treated with surgery alone at the same institution. The rate of 5-year survival was 34%.
Patients who achieved a histologic CR from the preoperative regimen had a median survival of 70 months, and 60% were alive at 5 years. However, patients with residual cancer in the esophagus at time of resection also achieved an improved median survival of 26 months, and 32% were alive at 5 years. This substantial increase in long-term survival among the patients with residual tumor in the resected esophagus suggests a continued benefit from esophagectomy. These pilot data served as the rationale for a randomized study recently completed at the University of Michigan Medical Center. The preliminary results of this randomized study will be discussed further in the next section on randomized trials.
Fox Chase StudySauter and colleagues[16] at Fox Chase Cancer Center used a preoperative regimen of 5-FU/mitomycin (Mutamycin)/radiotherapy in adenocarcinoma patients only.[16] They treated 30 patients with stage I or II disease with two cycles of continuous- infusion 5-FU, one cycle of mitomycin, and concurrent radiation to a total dose of 6,000 cGy. Of the 30 patients, 10 were unable to tolerate the entire regimen due to severe esophagitis. Surgical exploration was done in 21 patients; 18 patients underwent a curative resection, and, of these patients, 39% had a pathologic complete response.
There was a trend for improved survival in patients who had no residual tumor in the resected specimen. Rates of survival at 2 and 3 years for all patients were 33% and 25%, respectively. Median survival was better for those patients who underwent esophagectomy than for those who did not (23 vs 9 months), although the study was not designed to test this question in a randomized fashion.
Role of Preresection EsophagogastroduodenoscopyA study by Bates et al[17] at the University of North Carolina attempted to determine the role of preresection esophagogastroduodenoscopy in predicting which patients treated with chemoradiation could potentially forgo surgery. Thirty-five patients were treated with 5-FU, cisplatin, and radiation to a total dose of 4,500 cGy. The pathologic complete response was 51%.
Of the 35 patients, 22 (63%) underwent a preresection upper endoscopy with brushings and biopsies 1 to 3 days before the planned esophagectomy. Although 17 (77%) of the 22 patients had negative pathology from this evaluation, 7 (41%) of these 17 patients had residual tumor in the resected specimen. Therefore, the authors concluded that preresection endoscopy was not a reliable predictor of pathologic complete response. Esophagectomy appeared to contribute to the survival of this group, because 25% of patients with residual tumor in the resected esophagus were long-term survivors.
These nonrandomized trials show that patients who achieve a histologic complete response generally have better survival than those who have persistent disease in the esophagus after chemoradiation, and a complete response rate of at least 25% is a typical result from these regimens. Survival benefit from chemoradiation can only be demonstrated through randomized trials.
Randomized Studies
Two randomized studies[10,18] have evaluated sequential chemotherapy and radiotherapy followed by surgery, and three others[19-21] have evaluated concomitant chemoradiation.
Sequential ChemoradiationThe Norwegian trial reported by Nygaard et al[10] randomized patients with potentially resectable squamous-cell cancer to either (l) surgery alone, (2) preoperative chemotherapy with cisplatin and bleomycin, (3) preoperative radiation of 3,500 cGy, or (4) preoperative cisplatin and bleomycin, followed by radiation and then surgery. There was no significant difference in median, 3- or 5-year survival rates when the three sequential modalities were compared to treatment with surgery alone. Three-year survival was significantly higher in the pooled groups receiving radiotherapy compared to the groups not receiving radiotherapy.
The number of patients in the trial was relatively small for a four-arm randomized trial. Some differences in patient selection may have led to the apparent benefit rendered by radiation therapy, because a larger percentage of patients receiving radiotherapy had T1 lesions, and these patients with very early lesions may have done well no matter what treatment regimen they received. Also, more patients were lost to follow-up in the radiotherapy group (9%) than in the nonradiotherapy group (2.8%) and were excluded from analysis. Thus, the authors' conclusion that preoperative radiation may have a beneficial effect on intermediate survival must be viewed with caution.
LePrise and colleagues[18] from Rennes, France, conducted a randomized study of surgery vs preoperative chemoradiation in 86 evaluable patients with squamous-cell carcinoma. The chemotherapy consisted of cisplatin and 5-FU administered before and after the delivery of 2,000 cGy of radiation followed by surgery. The study was to enroll 150 patients to detect an improvement in 2-year survival, from 10% to 30%. However, the trial closed early after the accrual of 104 patients, because there was no significant survival difference at 1, 2, and 3 years.
The authors admitted that one of their main objectives was to avoid an increase in postoperative morbidity, and therefore, they chose to adopt a regimen that was not very aggressive. Thus, while this neoadjuvant treatment did not alter survival time, the intensity of the regimen was fairly mild.
Concomitant ChemoradiationA University of Michigan Medical Center randomized trial comparing surgery alone with an intensive 21-day regimen of concomitant chemotherapy and radiation was reported by Urba and colleagues.[19] The nonrandomized pilot data described in the previous section provided the rationale for this trial.[15] The chemoradiation consisted of cisplatin, vinblastine, and 5-FU administered with concurrent radiation to a total dose of 4,500 cGy. Patients were stratified according to tumor histology, size, and location.
A total of 100 patients were enrolled in the study, 50 patients on each arm. Approximately 75% of patients on each arm had adenocarcinoma. Forty-five patients on each arm underwent gross total resection of disease.
For patients pretreated with chemoradiation, the CR rate was 28%. At a median follow-up of 2.32 years, there was no difference in median survival (1.48 years for the surgery-alone arm and 1.46 years for the chemoradiation arm) or 2-year survival (39% and 42%, respectively). However, the study was designed to detect a large (100%) increase in survival between arms. Recent review of the data at a median follow-up of 3.78 years suggests that the survival curves may be separating, in favor of the chemoradiation arm.
The data will be formally assessed again within the year. Thus, at this time, no final conclusions regarding survival have yet been drawn from this trial.
Walsh and colleagues[20] from Ireland compared surgery with preoperative chemotherapy and radiation followed by surgery. In this randomized trial, 113 patients with adenocarcinoma received either surgery alone or multimodality therapy consisting of 5-FU, cisplatin, and radiation (4,000 cGy). The histologic CR rate was 25%.
An intention-to-treat analysis showed a survival advantage for the combined-modality group over the surgery group (median survival, 16 vs 11 months; P = .01). The 3-year survival rate also was significantly higher in the chemoradiation group than in the surgery group (32% vs 6%; P = .01).
The European Organization for Research and Treatment of Cancer (EORTC) recently completed a large randomized trial[21] comparing surgery alone with preoperative chemotherapy and radiation in 275 patients with stage I and II squamous-cell carcinoma of the esophagus. The regimen consisted of cisplatin and radiation, delivered with a 2-week break in the middle. The final report of this trial has not yet been published.
Of the three completely reported trials, two showed no survival benefit for chemoradiation over surgery, and one did demonstrate a survival advantage for patients with adenocarcinoma treated with preoperative chemoradiation. Confirmatory evidence depends on the forthcoming final results of the EORTC and University of Michigan trials.
There is no general consensus about the need for surgery in patients with localized disease. No randomized study has been successfully completed comparing patients treated with surgery with those treated with radiation or chemoradiation. However, three studies have tested radiation therapy alone vs chemotherapy and radiation in patients with esophageal cancer.
Randomized Studies
Brazilian StudyA trial from Rio de Janeiro randomized 59 patients with squamous-cell carcinoma to either 5,000 cGy of radiation (arm 1) or mitomycin and bleomycin given concurrently with radiation (arm 2).[22] There was no difference in survival between the groups. Rates of survival at 1, 2, and 3 years were 55%, 22%, and 6% in arm 1 and 64%, 38%, and 16%, respectively, in arm 2.
ECOG StudyThe Eastern Cooperative Oncology Group (ECOG) reported, in abstract form, the preliminary results of a randomized study[23] comparing radiation (4,000 cGy) alone vs radiation (4,000 cGy) combined with 5-FU and mitomycin in 119 patients with squamous-cell carcinoma of the esophagus. Patients then had the option of undergoing surgical evaluation. Those who did not have surgery received an additional 2,000 cGy of radiation.
Median survival was 14.8 months vs 9.1 months in favor of the chemoradiation arm (P = .03). The authors concluded that the combination of chemotherapy and radiation confers a survival advantage compared with radiation alone, and future trials should explore more intensive regimens of chemoradiation with or without surgery.
Intergroup TrialsA large Intergroup trial initiated by the RTOG enrolled 121 patients with esophageal cancer.[24] One treatment arm was radiation alone (6,400 cGy), and the second was 5-FU and radiation (5,500 cGy). Median survival for radiation-treated patients was 8.9 months, as compared with 12.5 months for patients treated with chemoradiation. Survival rates at 12 and 24 months were also significantly better for patients treated wit chemoradiation.
A recent abstract updating these results confirms that the survival differences persist.[25] With a minimum follow-up of 5 years for all patients, 5-year survival was 0% for the patients treated with radiation alone and 30% for the patients treated with chemoradiation (P < 0001). The chemoradiation arm was associated with a higher degree of toxicity.
A new Intergroup randomized trial, which opened in June 1995, is comparing high-dose radiation and chemotherapy vs conventional-dose radiation and chemotherapy. Projected accrual is 298 patients.
SummaryIt is clear that nonsurgical treatment is the best approach for patients with inoperable disease or those who are physically unable to tolerate surgery. For these patients, chemoradiation appears to be superior to radiation alone. However, for the patient healthy enough to tolerate surgery, the role of surgery in the treatment regimen tends to vary from institution to institution, and no randomized trials have directly compared surgery alone to radiation or chemoradiation. We favor the inclusion of surgery in the treatment regimen, because some patients who have persistent tumor in the resected esophagus after preoperative chemoradiation can become long-term survivors.
Some of the most promising data for patients with esophageal carcinoma who have potentially resectable disease come from studies that utilized concurrent chemoradiation in the preoperative setting. However, the positive randomized trial showing a survival advantage for preoperative chemoradiation involved only patients with adenocarcinoma and thus needs to be confirmed for patients with squamous-cell carcinoma. Also, in the near future, results from two other large randomized trials should become available and may further alter approaches to treatment.
Patients who are not operative candidates should be treated with chemotherapy combined with radiation if possible, because two randomized trials have demonstrated a survival advantage. However, concurrent treatment is more toxic, and it is therefore possible that frail patients may best be treated with single-modality therapy, according to the judgment of the physician.
Although no randomized trials have addressed the necessity of surgery as part of the treatment regimen for esophageal cancer, potentially resectable patients may benefit from the resection of disease that has been only partially eradicated by chemoradiation. As more randomized trial data become available in the future, guidelines for treatment of this disease will continue to evolve.
References:
1. Schottenfeld D: Epidemiology of cancer of the esophagus. Semin Oncol 11:92-100, 1984.
2. Yang PC, David S: Incidence of cancer of the esophagus in the U.S. by histologic type. Cancer 61:612-617, 1988.
3. Blot WJ, Devesa SS, Kneller RW, et al: Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA 265:1287-1289, 1991.
4. Wynder EL, Bross IJ: A study of etiological factors in cancers of the esophagus. Cancer 14:389-413, 1961.
5. Cameron AJ, Ott BJ, Payne WJ: The incidence of adenocarcinoma in columnar-lined
(Barrett's) esophagus. N Engl J Med 313:857-859, 1985.
6. Naef AP, Savary M, Ozzello L: Columnar-lined lower esophagus: An acquired lesion with malignant predisposition: Report on 140 cases of Barrett's esophagus with 12 adenocarcinomas. J Thorac Cardiovasc Surg 70:826-835, 1975.
7. Spechler SJ, Robbins AH, Rubins HB, et al: Adenocarcinoma and Barrett's esophagus: An overrated risk? Gastroenterology 87:927-933, 1984.
8. Roth JA, Pass HI, Flanagan MM, et al: Randomized clinical trial of preoperative and postoperative adjuvant chemotherapy with cisplatin, vindesine, and bleomycin for carcinoma of the esophagus. J Thorac Cardiovasc Surg 96:242-248, 1988.
9. Schlag PM: Randomized trial of preoperative chemotherapy for squamous cell cancer of the esophagus: The Chirurgische Arbeitsgemeinschaft für Onkologie der Deutschen Gesellschaft für Chirurgie Study Group. Arch Surg 127:1446-1450, 1992.
10. Nygaard K, Hagen S, Hansen HS, et al: Preoperative radiotherapy prolongs survival in operable esophageal carcinoma: A randomized, multicenter study of preoperative radiotherapy and chemotherapy. The second Scandinavian trial in esophageal cancer. World J Surg 16:1104-1109, 1992.
11. Seydel HG, Leichman L, Byhardt R, et al: Preoperative radiation and chemotherapy for localized squamous cell carcinoma of the esophagus: An RTOG study. Int J Radiat Oncol Biol Phys 14:33-35, 1988.
12. Poplin E, Fleming T, Leichman L, et al: Combined therapies for squamous-cell carci-
noma of the esophagus. A Southwest Oncology Group study (SWOG-8037). J Clin Oncol 5:622-628, 1987.
13. Naunheim KS, Petruska PJ, Roy TS, et al: Preoperative chemotherapy and radiotherapy for esophageal carcinoma. J Thorac Cardiovasc Surg 103:887-895, 1992.
14. Forastiere AA, Orringer MB, Perez-Tamayo C, et al: Concurrent chemotherapy and radiation therapy followed by transhiatal esophagectomy for local-regional cancer of the esophagus. J ClinOncol 8:119-127, 1990.
15. Forastiere AA, Orringer MB, Perez-Tamayo C, et al: Preoperative chemoradiation followed by transhiatal esophagectomy for carcinoma of the esophagus: Final report. J Clin Oncol 11:1118-
1123, 1993.
16. Sauter E, Coia L, Keller S: Preoperative high-dose radiation and chemotherapy in adenocarcinoma of the esophagus and esophagogastric junction. Ann Surg Oncol l:5-10, 1993.
17. Bates B, Detterbeck F, Bernard S, et al: Concurrent radiation therapy and chemotherapy followed by esophagectomy for localized esophageal carcinoma. J Clin Oncol 14:156-163, 1996.
18. LePrise E, Etienne P, Meunier B, et al: A randomized study of chemotherapy, radiation therapy, and surgery versus surgery for localized squamous-cell carcinoma of the esophagus. Cancer 73:1779-1784, 1994.
19. Urba S, Orringer M, Turrisi A, et al: A randomized trial comparing transhiatial esophagectomy to preoperative concurrent chemoradiation followed by esophagectomy in locoregional esophageal carcinoma (abstract). ProcAm Soc Clin Oncol 14:199, 1995.
20. Walsh T, Noonan N, Hollywood D, et al: A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med 335:462-467, 1996.
21. Bossett JF, Gignoux M, Triboulet JP, et al: Randomized phase III clinical trial comparing surgery alone vs preoperative combined radio-chemotherapy in stage I-II epidermoid cancer of the thoracic esophagus: Preliminary analysis, a study of the FFCD (French Group) no. 8805 and EORTC no. 40881 (abstract). Proc Am Soc Clin Oncol 13:576, 1994.
22. Araujo C, Souhami L, Gil R, et al: A randomized trial comparing radiation therapy vs concomitant radiation therapy and chemotherapy in carcinoma of the thoracic esophagus. Cancer 67:2258-2261, 1991.
23. Sischy B, Ryan L, Haller D, et al: Interim report of EST 1282 phase III protocol for the evaluation of combined modalities in the treatment of patients with carcinoma of the esophagus, stage I and II (abstract). Proc Am Soc Clin Oncol 9:105, 1990.
24. Herskovic A, Martz K, al-Sarraf M, et al: Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus. N Engl J Med 326:1593-1598, 1992.
25. al-Sarraf M, Martz K, Herskovic A, et al: Superiority of chemoradiotherapy vs. radiotherapy in patients with esophageal cancer. Final report of an Intergroup randomized and confirmed study (abstract). Proc Am Soc Clin Oncol 15:464, 1996.
- © 1997 by PRR, Inc. All rights reserved.
Articles in this issue
over 28 years ago
UFT: East Meets West in Drug Developmentover 28 years ago
Rationale for Phase I Study of UFT Plus Leucovorin and Oral JM-216over 28 years ago
Postoperative Adjuvant Chemotherapy for Non-Small-Cell Lung Cancerover 28 years ago
UFT in Gastric Cancer: Current Status and Future Developmentsover 28 years ago
Oral UFT and Leucovorin in Patients With Advanced Gastric CarcinomaNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.