- ONCOLOGY Vol 17 No 2
- Volume 17
- Issue 2
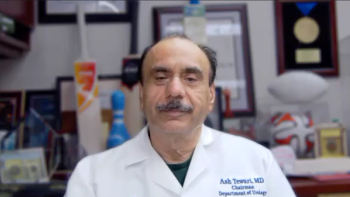
Commentary (Moul)-Testicular Cancer: Maintaining the High Cure Rate
Dr. Derek Raghavan, a recognizedexpert in the managementof testicular cancer, isto be congratulated for a clear andconcise overview of the contemporarymanagement of testicular cancer.As a urologist with almost 20years’ experience in the treatment oftesticular cancer, I fully agree withthe concept of not modifying or delayingthe use of proven treatmentprotocols.I can remember as an internand junior resident seeing youngcontemporaries die a horrible deathfrom testicular cancer. Any clinician40 years of age or older can relate tothis scenario, and it probably had thesame impact on them as it did onme-we don’t ever want to “gothere” again.
Dr. Derek Raghavan, a recognized expert in the management of testicular cancer, is to be congratulated for a clear and concise overview of the contemporary management of testicular cancer. As a urologist with almost 20 years' experience in the treatment of testicular cancer, I fully agree with the concept of not modifying or delaying the use of proven treatment protocols. I can remember as an intern and junior resident seeing young contemporaries die a horrible death from testicular cancer. Any clinician 40 years of age or older can relate to this scenario, and it probably had the same impact on them as it did on me-we don't ever want to "go there" again.
Recently, we experienced an unfortunate case of "patient-mediated" noncompliant surveillance that ultimately resulted in the patient's death. Our current crop of residents was completely unaccustomed to this event, unlike 20 years ago. I could not agree more with Dr. Raghavan that inappropriate surveillance of clinical stage I nonseminomatous germ cell tumor (NSGCT)-as the result of unstructured follow-up by clinicians or noncompliant and poorly selected patients-is potentially deadly.
Histopathologic Risk Factors
TABLE 1
Probability of Predicting Final Pathologic Stage in Patients With Stage I NSGCT Using Various Parameters
Although Dr. Raghavan has covered the issues of chemotherapy and late toxicity very well, I would like to add my urologic perspective on early-stage NSGCT. In particular, I would like to address the use of primary tumor histopathologic risk factors to stratify the risk of occult retroperitoneal metastases in men with clinical stage I NSGCT.
Our group has shown that the combination of the percentage of the embryonal carcinoma component and the presence or absence of vascular invasion in the primary tumor are powerful prognostic factors.[1] We have reported our updated experience with 149 clinical stage I NSGCT patients examining vascular invasion, percentage of embryonal carcinoma, p53 expression, bcl-2 expression, MIB-1 (Ki-67) expression, cathepsin D expression, and E-cadherin expression.[ 2] As in our prior work,[1] vascular invasion and percentage of embryonal carcinoma were the only primary tumor factors that predicted pathologic stage on multivariable analysis.
TABLE 2
Sensitivity, Specificity, and Predictive Values for Defined Cutoff Values in Predicting Final Pathologic Stage of NSGCT
We agree with Dr. Raghavan that it is of paramount importance to be able to identify clinical stage I NSCGT patients who are suitable for surveillance. To that end, our updated study in 149 patients identified this low-risk group using a threshold of ≤ 45% embryonal carcinoma and the absence of vascular invasion.[2] Table 1 provides the various cut points for percentage of embryonal carcinoma with or without vascular invasion, and Table 2 provides the sensitivity, specificity, and predictive values for these parameters. We feel it is important to carefully assess the primary tumor for vascular invasion and percentage of embryonal carcinoma and consider a percent embryonal cutoff of ≤ 45% to select patients at very low risk of occult metastases or recurrence.
Retroperitoneal Lymph Node Dissection
Another area of concern in the urologic surgical management of NSGCT is laparoscopic retroperitoneal lymph node dissection.[3-6] Although this relatively new surgical technique is being applied at some centers of excellence, it has not been compared in a randomized trial with the gold standard-open retroperitoneal lymph node dissection-nor has there been long-term follow-up sufficient to determine efficacy or to assess the ability to preserve ejaculatory function.
Financial Disclosure:The author has no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Moul JW, McCarthy WF, Fernandez EB, et al: Percentage of embryonal carcinoma and of vascular invasion predicts pathological stage in clinical stage I nonseminomatous testicular cancer. Cancer Res 54:362-364, 1994.
2. Heidenreich A, Sesterhenn IA, Mostofi FK, et al: Prognostic risk factors that identify patients with clinical stage I nonseminomatous germ cell tumors at low risk and high risk for metastasis. Cancer 83:1002-1011, 1998.
3. Gerber GS, Bissada NK, Hulbert JC, et al: Laparoscopic retoperitoneal lymphadenectomy: Multi-institutional analysis. J Urol 152:1188- 1191, 1994.
4. Nelson JB, Chen RN, Bishoff JT, et al: Laparoscopic retoperitoneal lymph node dissection for clinical stage I nonseminomatous germ cell testicular tumors. Urology 54:1064- 1067, 1999.
5. Rassweiler JJ, Frede T, Lenz E, et al: Long-term experience with laparoscopic retroperineal lymph node dissection in the management of low-stage testis cancer. Eur Urol 37:251-260, 2000.
6. Janetschek G: Laparoscopic retoperitoneal lymph node dissection. Urol Clin North Am 28:107-114, 2001.
Articles in this issue
about 23 years ago
Supportive Care in Cancer: A General Overviewabout 23 years ago
Special Considerations for Nutrition Intervention With Oncology Patientsabout 23 years ago
Smoking Cessation Help for the Elderlyabout 23 years ago
Second-Line Treatment of Small-Cell Lung Cancerabout 23 years ago
Commentary (Witta/Bunn): Second-Line Treatment of Small-Cell Lung Cancerabout 23 years ago
HHS Unites Its HIV AdvisorsNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.