Gut Bacteria Predict Responses, Survival Time to PD-1 Cancer Immunotherapy
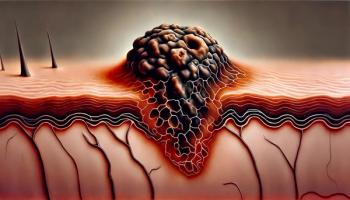
The gut microbiome affects the efficacy of PD-1 immune checkpoint blockade immunotherapy against melanoma and other cancers, according to a pair of recent studies.
The gut microbiome affects the efficacy of PD-1 immune checkpoint blockade immunotherapy against melanoma and other cancers, according to two studies published in Science.
“Our results indicate that the gut microbiome may modulate responses to anti–PD-1 immunotherapy in melanoma patients,” reported lead
Previously reported mouse studies suggested that the bacterial composition of the gut microbiome can modulate responses to anticancer immunotherapy, possibly explaining why mice purchased from different companies exhibit different responses to PD-1 inhibitors.
The new studies were undertaken to determine whether or not the composition of human gut microbiomes similarly modulates responses to PD-1–based immunotherapy in patients with melanoma or other cancers.
Gut bacteria diversity and composition indeed predicted PD-1 inhibitor responses among patients with melanoma, Dr. Wargo’s team reported. The team also examined oral microbiomes but found no baseline associations with treatment response.
Patients with more Ruminococcaceae-order and fewer Bacteroidales-order species experienced significantly better responses and had higher concentrations of circulating and tumor microenvironment immune T cells, Dr. Wargo’s team found. These patients also experienced longer progression-free survival times than did other patients.
An analysis of patient fecal microbiome samples in 30 responders and 13 nonresponders showed significantly higher alpha diversity (P < .01) and a relative abundance of Ruminococcaceae bacteria (P < .01) in responding patients.
“Metagenomic studies revealed functional differences in gut bacteria in [responders] including enrichment of anabolic pathways,” reported Dr. Wargo and coauthors. “Together, these data have important implications for the treatment of melanoma patients with immune checkpoint inhibitors.”
The
Both research teams also transplanted fecal microbiota from cancer patients to germ-free mice. Mice responded better to PD-1 inhibition after receiving fecal transplants from patients who had responded well to the immunotherapy, compared to mice receiving feces from patients who did not respond. Feeding A. muciniphila to the mice that had responded poorly to immunotherapy triggered subsequent responses, Dr. Zitvogel’s team found.
It is not yet clear what mechanisms account for the associations between gut bacteria and immunotherapy responses, but gut microbiota composition might prove to be a useful predictive biomarker for immune checkpoint inhibition, the authors noted.
Dr. Wargo and colleagues also suspect that manipulating the composition of patients’ microbiome might sensitize their immune systems to PD-1-based therapies. That team is planning a clinical trial to find out.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.