Oncology NEWS International
- Oncology NEWS International Vol 16 No 3
- Volume 16
- Issue 3
How to Bring Down the Burgeoning Costs of Cancer Imaging
Diagnostic imaging consumes about 3.6% of the total health care dollars nationally ($80 billion), and is growing steadily at about 18% per year.
Diagnostic imaging consumes about 3.6% of the total health care dollars nationally ($80 billion), and is growing steadily at about 18% per year. Cancer Care & Economics (CC&E) recently spoke with Brian Baker about this issue. Mr. Baker, vice president, Regents Health Resources, Inc., Brentwood, Tennessee, is a nationally recognized expert on developing and managing medical imaging services.
CC&E: Are we making progress developing radiotherapies that cause less damage to healthy tissue?
MR. BAKER: Absolutely. Accuracy is the key to optimizing patient outcomes. Advances in today's imaging technologies are being integrated into radiotherapy, and dramatically improving its accuracy.
In addition, we are seeing more interest in and utilization of particle, or proton, therapy. In its current form, particle therapy causes less collateral damage than traditional radiotherapy.
But the future is even more exciting. Pencil beam scanning is about 3 years away. It will further increase accuracy and reduce the time required to plan the therapy. It works by giving the radiotherapist precise control of a very small beam.
CC&E: Proton therapy units cost upward of $125 million. How can a medical facility expect a return on such a huge investment?
MR. BAKER: There are options now to get systems implemented more easily. Ion Beam Applications (IBA) of Belgium just won a $30 million contract for the first single-gantry proton therapy system in the United States. That's easier to swallow than $125 million for a four-gantry proton therapy center.
This approach lets an organization service the clinical need and add capability as need grows. Even better, proton therapy reimbursement increased by about 22% last year. So somebody sees value; otherwise, the reimbursement wouldn't rise.
A single-gantry proton therapy system can treat between 300 and 400 patients a year, assuming 30 to 40 treatments per patient. The average reimbursement for a simple visit is about $1,100 whereas complex visits average about $1,300.
Without considering the operational costs that vary from program to program, you're looking at about a 3-year payoff on a single-gantry system.
Considering the potential benefits conferred by proton therapy, which causes less damage to healthy tissue, these single-gantry proton therapy units represent a good option.
CC&E: Should the burden of seeing that imaging technologies are used efficiently fall primarily on the shoulders of the imaging management companies?
MR. BAKER: It's a burden that should be spread across the healthcare community. The trick is to put in a system of scientifically based checks and balances that works to the advantage of everyone in health care and that reduces redundancy and waste.
The imaging management companies are charged with defining appropriateness, in terms of utilization as well as credentialing the imaging provider and the imaging tools. In the future, imaging management companies will likely also focus on the match between a device's capabilities and the clinical indications that it can evaluate.
CC&E: How can we integrate imaging and treatment technologies in a more complementary way?
MR. BAKER: With information technology (IT) and protocols. If we want to more efficiently implement, track, and modify our cancer treatment plans, we have to solve the diagnostic-treatment disconnect. The question is: "How do we accurately and efficiently use informational crosstalk to translate the imaging information from a diagnostic to a treatment modality?"
Diagnostic information is used very differently than the information gathered just prior to treatment. The goals are different, and so are the viewpoints of the scientists within those disciplines. And in some cases, the financial incentives are different, too.
In addition to overcoming the technology hurdles, we have to more closely integrate the processes of the primary care physician, the radiologist, and the oncologist. The IT integration is already happening.
CC&E: Imaging technologies are often cast as the bad guys in our burgeoning healthcare budget. Is this an unfair assessment?
MR. BAKER: Yes, I think it is unfair. Imaging payments have absorbed a disproportionate share of payer resources. But this makes sense. Most experts agree that imaging technology advances are providing greater opportunities to diagnose disease. As the population ages, so does our need for additional diagnosis and cancer care. These two elements alone are reason enough for increased utilization.
There's less agreement about why physicians order imaging examinations. Unfortunately, a lack of knowledge about these technologies may drive some inappropriate utilization. However, in the near future we'll see more education and clever decision support tools that help physicians match indications to the best equipment and procedures.
CC&E: How can the community oncologist compete in this costly market?
MR. BAKER: The community oncologist must have a strong business plan and must focus on collaboration with other physicians. Being independent makes it expensive to compete and hard to succeed in today's marketplace. Strategic partnerships can solve this by spreading risks and aligning goals. Diversifying is another way to spread the risk. Oncology partnerships that incorporate complementary specialties can be very productive. They are like a marriage, in a way, except that more money is typically involved and more waking hours are spent together. Before you commit to any partnership opportunity, give it at least as much preparation, thought, and attention as you devoted to your marriage.
CC&E: Where do you see radiotherapy in the next 10 years?
MR. BAKER: I foresee closer integration of imaging and treatmentsystems that require less set-up time, are more accurate, and produce less collateral damage. As advanced imaging applications such as CAD (computer-aided diagnostics) are perfected and combined with advances in IT, imaging technology will become more automated. These integrated systems will provide more real-time feedback to the physician, which, in turn, will enhance accuracy by allowing changes during treatment.
The breakthrough that will really catapult us into the future will be a "best of breed" common IT platform and interface. A standard communication protocol will interface all imaging modalities with advanced treatment planning and therapy. So as the patient moves and as the malignancy changes in response to treatment, the therapy will be modified in real time. All these advances will be combined with or used to activate targeted drug therapies as well.
Articles in this issue
almost 19 years ago
Peptide-Based Breast Ca Vaccines Promising in Early Trialsalmost 19 years ago
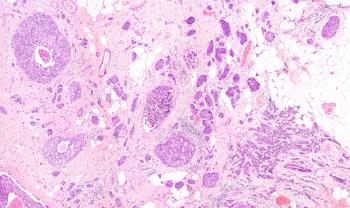
Diagnostic Dilemma: GI Diseasealmost 19 years ago
Imatinib Responses in CML May Take Timealmost 19 years ago
IV Vidaza Approved; Oral Formulation to Be Testedalmost 19 years ago
Study Confirms Avastin Advantage in Advanced NSCLCalmost 19 years ago
Legal Services Should Be a Component of Standard Cancer Carealmost 19 years ago
Mouse Virus Evidence Suggests Viral Basis for Breast Caalmost 19 years ago
Groups Oppose Ruling on Access to Experimental Drugsalmost 19 years ago
Satellite Allows Digital Mammography Screening for Rural Native Americansalmost 19 years ago
Nexavar Effective in Advanced HCC: Phase III Trial StoppedNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.