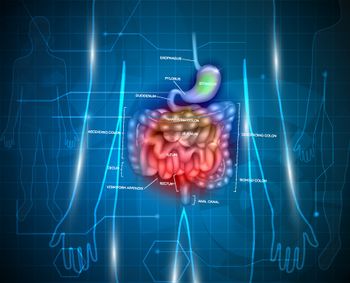
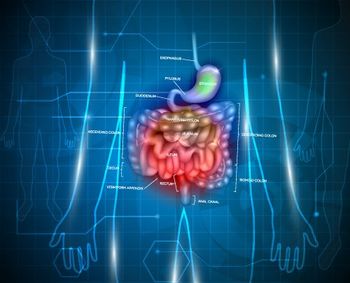
Neuroendocrine tumors (NETs) are a broad family of tumors classified by site of origin and histologic characteristics. Per a Surveillance, Epidemiology and End Results (SEER) database analysis, the incidence of NETs in the United States was estimated to be 5.25/100,000 in 2004; this was likely an underestimation, given that these tumors often go unreported or undiagnosed.[1] Bronchial carcinoids account for 25% to 30% of all NETs, while gastroenteropancreatic (GEP) NETs account for 65% to 70%. Within the GI tract, the most common sites of origin are the small bowel (including appendix), stomach, and rectum.Rarely, the thymus and other sites may also be affected.[1,2]
Accumulating evidence shows that pancreatic NETs are biologically and clinically distinct from other NETs and therefore should not be grouped together with the latter. Also, the term “carcinoid” should not be used to describe pancreatic NETs, although it is used for other NETs. Based on tumor differentiation, the 2010 World Health Organization classification grouped NETs into well-differentiated (low- or intermediate-grade) or poorly differentiated (high-grade) tumors. Although considerable debate continues regarding the most clinically relevant cutoffs for this classification, GEP NETs with a mitotic index of < 2 mitoses per 10 high-power fields (HPF) and a Ki-67 index of < 3% are deemed to be low grade, and NETs with a mitotic index of 2–20 mitoses per 10 HPF and a Ki-67 index of 3% to 20% are intermediate grade. Lung and thymic carcinoids are considered to be either typical, with a mitotic index of < 2 mitoses per HPF and with no necrosis, or atypical, with a mitotic index of 2–10 mitoses per HPF and with noted foci of necrosis. NETs with a higher mitotic index and/or Ki-67 index are classified as high grade or poorly differentiated.[3] NETs may be functional, producing hormones that cause symptoms such as the classic carcinoid syndrome (intermittent facial flushing, diarrhea), or in the case of pancreatic NETs, symptoms attributable to an excess of insulin, glucagon, gastrin, or other peptides. NETs may also be asymptomatic or nonfunctional. Thus, the management of NETs is two-pronged, focusing on alleviation of symptoms in the case of functional tumors, and on the control of oncologic progression in all patients.
Surgical (or endoscopic, when feasible) resection is the treatment of choice for most locoregional NETs. In the case of intestinal carcinoids, surgical resection of the bowel, regional lymphadenectomy, and careful examination of the entire bowel is recommended to look for additional lesions. In the case of appendiceal and rectal carcinoids removed by simple appendectomy or endoscopy, respectively, additional surgery is recommended in the presence of poor prognostic features, including lymphovascular invasion and atypical histologic features, and/or for tumors larger than 2 cm. In patients with oligometastatic disease, resection of all visible disease is associated with prolonged survival, but the disease will recur in the majority, typically within 5 years.[3,4] Whether the improved outcome is due to selection of good-prognosis patients for surgery or to the debulking effect of resection cannot be ascertained without prospective, controlled studies. Treating physicians must also be aware of other potential local complications of small bowel NETs, including bowel obstruction due to a large primary lesion, traction of the mesentery, or ischemia due to vascular compromise from regional lymphadenopathy, which may require surgery. Also, carcinoid heart disease is an underappreciated complication and should be considered in carcinoid syndrome patients with cardiac symptoms and those undergoing surgical procedures.
All patients with symptoms secondary to hormone production should be started on a somatostatin analog at diagnosis. A recent analysis leveraging data from the SEER-Medicare database suggests that patients with carcinoid syndrome may be undertreated, especially early in the course of illness in elderly patients. Furthermore, undertreatment appears to be associated with inferior survival.[5] Of the available somatostatin analogs (lanreotide, octreotide, and pasireotide), only octreotide (available in a long-acting release [LAR] formulation given intramuscularly [IM] once a month, or in short-acting formulations for breakthrough symptoms) is currently approved by the US Food and Drug Administration (FDA) for control of hormonal symptoms associated with NETs. Patients may require short-acting octreotide in addition to octreotide LAR, typically 100–250 μg up to 3 times per day for breakthrough symptoms, especially for the first 10 to 14 days after LAR injection while awaiting therapeutic levels. In patients with progressive or poorly controlled symptoms, somatostatin analog doses may be increased as needed; liver-directed therapy, such as radiofrequency ablation, radioembolization, chemoembolization, and rarely surgical debulking, may also be considered as required.
Caution should be exercised in patients receiving IM somatostatin analogs, such as octreotide LAR, to ensure proper technique. In a study conducted by our group, up to 50% of injections were potentially delivered inappropriately, forming subcutaneous deposits that were picked up on CT scans.[6] Also, patients may continue to have diarrhea while receiving somatostatin analogs; it should be remembered that this might be due to factors other than carcinoid syndrome-such as prior bowel resections, autonomic dysfunction due to previous surgeries, and exocrine pancreatic insufficiency caused by octreotide (which can be managed with pancreatic enzyme supplements, such as pancrelipase capsules). Systemic therapy for tumor control of unresectable metastatic lung, GI, and pancreatic carcinoid tumors varies significantly. Thus, in patients with NETs of unknown primary (up to 13% of all NET patients per a SEER database study), attempts should be made to identify the origin of the neoplasm, guided by tumor histology, imaging, and/or endoscopy (especially to establish whether or not a patient has a primary pancreatic NET) to help guide treatment decisions.[1] There is controversy regarding the optimal time for initiation of therapy for oncologic control (at diagnosis vs at progression). Such decisions are based on analysis of potential risks and benefits. In our practice, we tend to follow patients with low-volume, indolent disease closely, with periodic scans, and initiate therapy at progression. Those with high-volume tumors and/or more aggressive clinical courses who may be at risk for developing symptoms or organ dysfunction with progression are offered therapy immediately.
GEP NETs
Based on the phase III PROMID study that showed benefit with octreotide LAR over placebo in patients with small bowel carcinoids, with regard to the primary endpoint of time to progression (14.3 months vs 6 months; P = .000072), the role of somatostatin analogs was well-established for disease control.[7] The recently concluded CLARINET trial extended the use of somatostatin analogs to the broader group of GEP NETs, as it showed benefit in progression-free survival (PFS) with lanreotide as compared with placebo in this patient population (not reached vs 18 months; P = .002), although the majority of patients had pancreatic NETs or small bowel carcinoids.[8] Lanreotide (given via deep subcutaneous injection once a month) is currently awaiting FDA approval for this indication based on these results; since it is given via deep subcutaneous injection, it is a potential option for patients who may have difficulties with octreotide LAR IM injections. Although interferon is a potential salvage therapy option after failure of somatostatin analogs for carcinoid patients, its use is limited, given its side effect profile. The phase III RADIANT-2 trial that randomized patients with progressive, functional carcinoid tumors to octreotide LAR with or without the mammalian target of rapamycin (mTOR) inhibitor everolimus demonstrated a 5.1-month improvement in median PFS with the addition of everolimus. However, this improvement did not meet the predefined threshold for statistical significance; thus, everolimus is currently not FDA-approved for the treatment of functional carcinoid tumors.[9] Data from the same study also showed that the addition of everolimus to octreotide significantly decreased hormonal secretion. Results of the RADIANT-4 study (NCT01524783), which has completed accrual, will help address the role of everolimus in nonpancreatic NETs of intestinal and pulmonary origin.[9] Our preference is to enroll patients with nonpancreatic GI NETs whose disease has progressed on somatostatin analogs in clinical trials when possible.
While pancreatic NETs have a more aggressive clinical course, recent advances have provided additional important treatment options that are altering the natural history of this disease. Large placebo-controlled phase III studies of patients with pancreatic NETs have shown improvement in PFS with targeted agents such as everolimus (11 months vs 4.6 months; P < .001) and the multi–tyrosine kinase vascular endothelial growth factor (VEGF) inhibitor sunitinib (11.4 months vs 5.5 months; P < .001).[10,11] Retrospective and small, prospective randomized studies suggest that pancreatic NETs also respond to cytotoxic chemotherapy: an MD Anderson Cancer Center series showed response rates up to 39% with fluorouracil, doxorubicin, and streptozocin.[12-14] Smaller series have suggested activity for temozolomide in combination with multiple agents; however, temozolomide has never been prospectively evaluated as a single agent. Its role is currently being explored in the randomized phase II Eastern Cooperative Oncology Group (ECOG) 2211 trial (temozolomide vs temozolomide and capecitabine; NCT01824875).
We typically choose therapy based on the clinical scenario. For instance, patients with high-volume disease or borderline resectable pancreatic NETs are offered upfront chemotherapy to debulk, while other patients are offered either a somatostatin analog or a targeted agent, depending on their comorbidities and the side-effect profile of the drug. Sunitinib is associated with hypertension, reflecting its anti-VEGF activity, while everolimus may cause hyperglycemia; thus, patients with uncontrolled diabetes mellitus may be started on sunitinib, while those with hypertension may be better suited for therapy with everolimus. In contrast to pancreatic NETs, other GI carcinoids are not responsive to chemotherapeutic agents, which are not typically used in those settings.
Key Points in the Initial Treatment of Well-Differentiated Neuroendocrine Tumors (NETs)
- In patients with unresectable, advanced well-differentiated NETs, management includes symptom and oncologic control. All patients with symptoms caused by hormone production should be started on a somatostatin analog (SSA) at diagnosis and continued on it indefinitely.
- Somatostatin analogs also have antitumor effects in gastroenteropancreatic NETs, resulting in significant improvement in progression-free survival; however, their role in the oncologic control of thoracic NETs is unclear.
- Pancreatic NETs are a distinct subgroup of NETs for which there are multiple additional therapeutic options, including targeted agents (sunitinib and everolimus) and conventional chemotherapeutic regimens based on streptozocin or temozolomide. In nonpancreatic NETs, however, there is no proven role for these agents
- Peptide receptor radionuclide therapy and liver-directed therapies, such as transarterial embolization, transarterial chemoembolization, and transarterial radioembolization, are other emerging therapeutic options.
Bronchial and Thymic Carcinoids
In contrast to GEP NETs, there are no guidelines to help direct therapy of advanced bronchial and thymic carcinoids. Chemoradiation has been suggested as a possibility in locally advanced, unresectable cases. However, in a retrospective SEER database analysis of thymic carcinoids, radiation did not show any survival benefit. In fact, the overall survival was significantly worse in patients who received radiation. This may have been due to selection bias, with patients with more advanced disease or incomplete resection more likely to receive radiation.[15] Patients with progressive, metastatic disease have been treated with somatostatin analogs, chemotherapeutic agents such as platinum-based therapy or temozolomide, or targeted agents such as everolimus or bevacizumab in small case series and trials; however, none of these agents have been tested in randomized trials. The ongoing LUNA trial (NCT01563354) is comparing pasireotide LAR, everolimus, or the combination in lung and thymic NETs.
Other Treatment Options
Transarterial approaches, such as transarterial embolization, transarterial chemoembolization, and transarterial radioembolization, are options that may be useful for symptom and disease control in patients with diffuse, unresectable liver-predominant disease. However, randomized trials evaluating these modalities are lacking. Peptide receptor radionuclide therapy (PRRT) is an experimental therapy based on the high prevalence of somatostatin receptors on NET cells, and has shown benefit in single-arm studies. Randomized trials, including NETTER-1 (lutetium-177–based PRRT vs high-dose octreotide in patients with progressive mid-gut NETs; NCT01578239) and CASTOR (PRRT vs interferon in nonpancreatic GI NETs with resistance to somatostatin analogs; NCT01860742), will provide more information regarding the efficacy and safety of this approach.
Conclusion
The management of NETs requires an adequate pathology review to determine the differentiation and grade of the tumor, followed by an assessment for curative resection. In patients with advanced, unresectable NETs, there are several treatment options; which of these may be considered depends on the site of origin of the tumor. Consider a somatostatin analog in all patients with advanced functional tumors. Recent data suggest that somatostatin analogs delay oncologic progression in GEP NETs. Everolimus and sunitinib have both shown robust benefit for patients with advanced pancreatic NETs. Cytotoxic chemotherapy in pancreatic NETs should be reserved for patients with bulky, symptomatic, or progressive disease. The role of everolimus in nonpancreatic NETs is being evaluated by the RADIANT-4 study.
Financial Disclosure: Dr. Yao serves as a consultant for Novartis and Ipsen, and has received research support from Novartis. Dr. Dasari has no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26:3063-72.
2. Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97:934-59.
3. Clark OH, Benson AB, 3rd, Berlin JD, et al. NCCN Clinical Practice Guidelines in Oncology: neuroendocrine tumors. J Natl Compr Canc Netw. 2009;7:712-47.
4. Glazer ES, Tseng JF, Al-Refaie W, et al. Long-term survival after surgical management of neuroendocrine hepatic metastases. HPB (Oxford). 2010;12:427-33.
5. Shen C, Shih YC, Xu Y, Yao JC. Octreotide long-acting repeatable use among elderly patients with carcinoid syndrome and survival outcomes: a population-based analysis. Cancer. 2014;120:2039-49.
6. Boyd AE, DeFord LL, Mares JE, et al. Improving the success rate of gluteal intramuscular injections. Pancreas. 2013;42:878-82.
7. Rinke A, Müller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27:4656-63.
8. Caplin ME, Pavel M, Cwikla JB, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371:224-33.
9. Pavel ME, Hainsworth JD, Baudin E, et al. Everolimus plus octreotide long-acting repeatable for the treatment of advanced neuroendocrine tumours associated with carcinoid syndrome (RADIANT-2): a randomised, placebo-controlled, phase 3 study. Lancet. 2011;378:2005-12.
10. Yao JC, Shah MH, Ito T, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364:514-23.
11. Raymond E, Dahan L, Raoul JL, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med. 2011;364:501-13.
12. Kouvaraki MA, Ajani JA, Hoff P, et al. Fluorouracil, doxorubicin, and streptozocin in the treatment of patients with locally advanced and metastatic pancreatic endocrine carcinomas. J Clin Oncol. 2004;22:4762-71.
13. Moertel CG, Lefkopoulo M, Lipsitz S, et al. Streptozocin-doxorubicin, streptozocin-fluorouracil or chlorozotocin in the treatment of advanced islet-cell carcinoma. N Engl J Med. 1992;326:519-23.
14. Moertel CG, Hanley JA, Johnson LA. Streptozocin alone compared with streptozocin plus fluorouracil in the treatment of advanced islet-cell carcinoma. N Engl J Med. 1980;303:1189-94.
15. Gaur P, Leary C, Yao JC. Thymic neuroendocrine tumors: a SEER database analysis of 160 patients. Ann Surg. 2010;251:1117-21.