New Combo Therapy Shows Promise in Leukemia
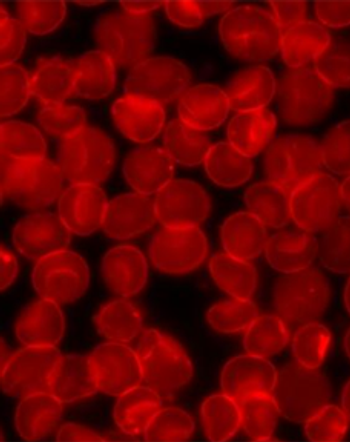
Leukemia cells show sensitivity to restriction of BCL2 and BTK with the combination of venetoclax and ibrutinib.
Inhibiting both Bruton's Tyrosine Kinase (BTK) and B-cell lymphoma 2 (BCL2) with ibrutinib and venetoclax showed promise in treating myeloid and lymphoid leukemia, according to the results of a study (
Genetic and epigenetic variability make the identification of targeted therapies for cancer challenging. Large-scale sequencing studies have demonstrated a gamut of mutations in cancer, meaning that combinations of agents are needed for treatment. “Combinatorial approaches will also be critical for combating the emergence of genetically heterogeneous subclones, rescue signals in the microenvironment, and tumor-intrinsic feedback pathways that all contribute to disease relapse,” wrote the authors.
The investigators utilized a functional ex vivo screening assay to identify small-molecule targeted inhibitors and inhibitor combinations showing selective efficacy vs broad categories of leukemia. They isolated primary mononuclear cells from 588 leukemia patients and plated these samples in the presence of a panel of more than 120 single-agent inhibitors or combinations representing several drug classes. The combinations were drug pairs that targeted non-overlapping biological pathways and consisted of different classes of drugs. The team determined IC50 and area under the curve (AUC) values using probit-based regression for each response curve. Disease status was based on chart review. Single and combination drug treatment IC50 and AUC values were compared within groups via statistical analysis.
In 588 leukemia patients, the team discovered that the combination of venetoclax and ibrutinib was more beneficial than either agent on its own for malignancies such as acute myeloid leukemia (AML), acute lymphoblastic leukemia, and chronic lymphocytic leukemia. Expanded analyses of combination sensitivity in AML patients demonstrated no significant links with age, gender, or European LeukemiaNet (ELN) prognostic risk. When comparing samples using disease-treatment status, the researchers found a marginally increased sensitivity in samples obtained from patients with relapsed/refractory AML (n=42) vs newly diagnosed AML (n=115), as indicated by both AUC and IC50 (P = .028 and .026, respectively). Using an expanded combination matrix involving AML cell lines, the team observed synergy with respect to most drug-pair concentrations.
“Both myeloid and lymphoid-derived primary leukemia cells show sensitivity to [the] combined inhibition of BCL2 and BTK with the combination of venetoclax and ibrutinib, suggesting this drug pair may have broad therapeutic indications,” concluded the authors.
In an exclusive interview with Cancer Network,
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.