Oncology NEWS International
- Oncology NEWS International Vol 5 No 3
- Volume 5
- Issue 3
No Adverse Effects of HRT on Breast Cancer Prognosis Seen
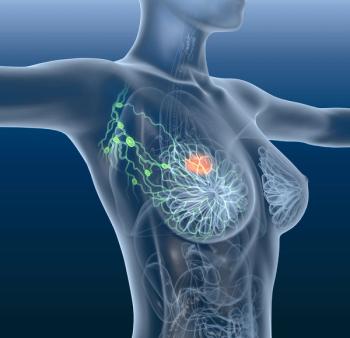
SAN ANTONIO--Three studies reported at the San Antonio Breast Cancer Symposium show no apparent adverse effects of hormone replacement therapy (HRT) on breast cancer and, in fact, suggest that breast cancers in patients with a history of HRT may have a more favorable prognosis in terms of histologic grade and estrogen-receptor (ER) levels.
SAN ANTONIO--Three studies reported at the San Antonio BreastCancer Symposium show no apparent adverse effects of hormone replacementtherapy (HRT) on breast cancer and, in fact, suggest that breastcancers in patients with a history of HRT may have a more favorableprognosis in terms of histologic grade and estrogen-receptor (ER)levels.
The largest study focused on 432 postmenopausal women diagnosedwith invasive breast cancer at University Hospital of South Manchester,England--109 with a history of HRT (mean duration, 48 months)and 323 who had never received hormones. To qualify as HRT users,patients must have used HRT for at least 3 months and within 3months of the cancer diagnosis, said surgical oncologist ClaudiaHarding.
Tumors in the two patient groups were similar with respect tonodal involvement, tumor size, and ER status. However, women whoreceived HRT had significantly more grade 1 tumors (42% vs 24%).A subanalysis showed that women who had taken hormones for morethan 2 years were significantly more likely to have ER-positivetumors.
"HRT is associated with better grade, and better grade isassociated with improved prognosis," Dr. Harding said. "Thus,HRT does not appear to have an adverse effect on mortality."She added that the similarity with respect to tumor size and nodestatus reflected that the women all had asymptomatic disease thatwas detected by screening.
Higher ER Levels
A Cincinnati study showed that hormone users develop tumors withsignificantly higher ER levels. Researchers evaluated the historyof hormone use (contraceptives, fertility drugs, and conjugatedestrogens) in 128 premenopausal and 197 postmenopausal women withbreast cancer. Overall, 102 patients had never used hormones forany purpose. Their breast tumors had a mean ER level of 51 fm/mgand a progesterone receptor (PR) level of 92.9 fm/mg.
By comparison, the 223 patients with a history of hormone usehad tumors with a significantly higher ER level, averaging 79.2fm/mg, and similar average PR level (107.9 fm/mg), reported ElyseLower, MD, associate professor of medicine, University of Cincinnati.
Separate analyses of pre- and post-menopausal women showed nosignificant correlations between hormone use and receptor levelsof tumors. Dr. Lower suggested that higher ER content might accountfor previous reports that post-menopausal hormone users developtumors with a more favorable prognosis.
Hormone therapy had no impact on histologic grade, tumor size,or nodal involvement in 161 symptomatic breast cancer patientsevaluated at the University of Liverpool, England. The populationincluded 29 patients receiving hormone therapy. "Women canthus be reassured that even if they do develop a primary breastcancer while taking HRT, this will not have an adverse effect,"said surgical oncologist Chris Holcombe.
Articles in this issue
about 30 years ago
Drug Allows Higher Doxorubicin Doses in Breast Ca Patientsabout 30 years ago
Nori Appointed to Cornell Department of Radiation Oncologyabout 30 years ago
Academic Centers Must Change or Perish in Climate of Managed Careabout 30 years ago
Genetically Altered Hematopoietic Cells Used in Transplant Researchabout 30 years ago
Bill Would Ease Distribution of Off-Label Dataabout 30 years ago
New Drug Combinations May Improve Outlook in AIDS Patientsabout 30 years ago
Dose-Intense Chemo in Breast Ca Questionedabout 30 years ago
LHRH Agonist Matches Ovariectomy Results: SWOGNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.