Recurrence and Relapse in Testicular Cancer
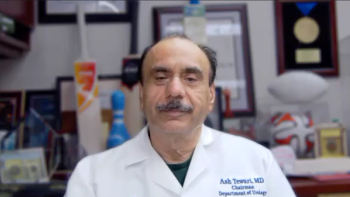
Dr. Bruce Roth, Siteman Cancer Center, spoke at the 2013 ASCO meeting about topics in seminoma. Here he discusses recurrence, relapse, and seminomatous vs nonseminomatous testicular cancer.
Dr. Bruce Roth, Professor of Oncology in the Division of Medicine at Siteman Cancer Center, Washington University at St. Louis, spoke with CancerNetwork at the 2013 ASCO meeting about topics in seminoma. Here he discusses recurrence, relapse, and seminomatous vs nonseminomatous testicular cancer.
Cancer Network: More than 80% of men with clinical stage I seminoma of seminoma are cured with orchiectomy alone, while 15% to 20% will have a recurrence if given no further treatment. In your practice, how do you manage a recurrence?
Dr. Roth: Recurrent disease in my practice is managed by giving the patient systemic chemotherapy. I think that we can see, from the [Mortenson, abstract 4502] presentation today, that even patients who are treated late with radiation therapy for a relapse, there’s still a relapse rate after that, and patients end up getting both chemotherapy and radiation treatment, and the side effects from both. So, I think recurrent disease is probably best treated with systemic chemotherapy.
Cancer Network: Is there a typical period for late relapse?
Dr. Roth: Late relapse is defined as [relapse] beyond 2 years from the initial diagnosis, but the pattern of relapse changes a little bit, as we saw today, based on the presence or absence of factors like lymphovascular invasion. Those patients tend to recur a little more quickly than patients without lymphovascular invasion, who are more likely to recur in the 2- to 5-year range.
Cancer Network: Dr. Mortenson also mentioned that three patients who had died were found to have non-seminomatous tissue. Could you talk a little bit about, clinically, the difference in terms of outcome with non-seminomatous tumors?
Dr. Roth: Patients with seminoma, basically when they recur, they’re treated with the same chemotherapy. If anything, they’re more chemosensitive than non-seminomatous germ cell tumors that recur, but usually the difference is in the treatment of early-stage disease. So, for patients that have undergone active therapy in the past, because of the radiosensitivity of seminoma, patients with clinical stage I would sometimes be offered low-dose radiotherapy to the retroperitoneum and pelvis, as adjuvant therapy, if you will; whereas those dose of radiation therapy would have no impact on non-seminomatous disease. Frequently, patients are quote “pure seminoma,” have normal markers, a few pathology slides are read as pure seminoma-but what they really have is a mixed germ cell tumor, with some elements of non-seminoma, and if you treat them, then sometimes you’ll find elements of non-seminoma down the road.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.