Oncology NEWS International
- Oncology NEWS International Vol 19 No 3
- Volume 19
- Issue 3
Single-shot Zevalin presents new lymphoma Rx option
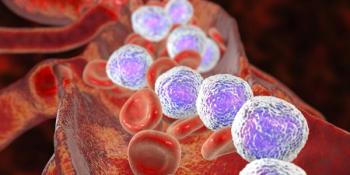
Unlike conventional radiation, Yttrium-90-ibritumomab tiuxetan (Zevalin) induces cellular damage only in the targeted tumor cells and has demonstrated activity in follicular and diffuse large B-cell non-Hodgkin’s lymphoma.
Unlike conventional radiation, Yttrium-90-ibritumomab tiuxetan (Zevalin) induces cellular damage only in the targeted tumor cells and has demonstrated activity in follicular and diffuse large B-cell non-Hodgkin's lymphoma. As a result, investigators in Italy were prompted to try radioimmunotherapy with Y-90-ibritumomab tiuxetan in extranodal marginal zone lymphoma, a disease that currently has no standard treatment after primary therapies fail.
"We saw superior rates of complete response and duration of response with Y-90-ibritumomab tiuxetan compared with those observed in extranodal marginal zone lymphoma (EMZL) treated with chemotherapy, monoclonal antibody alone, and combinations of the two," said Anna Vanazzi, MD, from the European Institute of Oncology in Milan. "If we can confirm these results in a larger trial, a single shot of Y-90-ibritumomab tiuxetan could be a valid option for treatment of relapsed EMZL."
The multicenter pilot phase II study enrolled 28 patients (median age 57) with relapsed/refractory marginal zone, CD-20-positive non-Hodgkin's lymphoma at any extranodal site. Fifteen patients had stage I-II disease and 13 had stage III-IV. Helicobacter pylorinegative gastric malt lymphoma was found in 12 patients and nongastric EMZL in 16. Patients had received a median of one prior regimen.
Primary endpoints were response rate (RR), duration of response (DOR), and overall survival (OS). Patients were pretreated with rituximab (Rituxan; 250 mg/mq), followed one week later by a similar dose of rituximab coupled with Y-90-ibritumomab tiuxetan (14.8 MBq/kg to a maximum dose of 1,184 MBq).
A 72% complete response (CR) was achieved in this group of refractory/ relapsed patients. Partial response was documented in 16% and stable disease in 12%. All patients were alive at the time the study was reported. Median DOR was not yet reached at the time of this presentation (ECCO/ESMO 2009 abstract O-9207).
At a median follow up of 26 months, duration of response ran from five months to 64 months in patients who maintained CR. Dr. Vanazzi said that six of 18 CRs have been kept up for more than three years.
Toxicities were primarily hematologic and reversible, she said. Fourteen patients developed grade 3 and 4 neutropenia, and the same group of patients developed grade 3 and 4 thrombocytopenia. Grade 3 anemia was seen in two patients.
Nonhematologic toxicity included one case of febrile neutropenia, one patient with herpes zoster infection, and two with fever of unknown origin; one case of perforated diverticulitis and one case of gastroenteritis occurred about 3 months after radioimmunotherapy, probably not related to the treatment received.
Radioimmunotherapy proves detrimental to stem cell mobilization
Dr. Vanazzi and colleagues presented a study at ASH 2009 that found pretreatments with purine analogues or Y-90-ibritumomab tiuxetan were independent factors that affected peripheral blood stem cell (PBSC) mobilization.
They retrospectively reviewed four years of data from their institution and evaluated the number of CD34+ cells after mobilization. The main mobilization regimen in hematologic patients was cyclophosphamide (4 g/mq) and ESHAP followed by G-CSF or by pegylated G-CSF; the majority of patients affected by solid tumors received ICE regimen plus G-CSF (abstract 3210).
Patients were labeled good mobilizers (peripheral CD34+ ≥ 20/μL), relatively poor mobilizers (peripheral CD34+ counts < 20 and ≥ 8/μL), and absolute poor mobilizers (peripheral CD34+ counts < 8/μL).
According to the results, 65.7% of patients were good mobilizers, 17.3% were relatively poor mobilizers, and 17% were absolute poor mobilizers. Independent risk factors affecting PBSC mobilization were three or more previous chemotherapy lines before mobilization (P < .001), and pretreatment with purine analogues (P = .007) or Y-90-ibritumomab tiuxetan (P = .0002). In a multivariate analysis purine analogs (P = .019) and 90-Y-ibritumomab tiuxetan (P = .003) were confirmed as detrimental.
Articles in this issue
almost 16 years ago
Final-Phase Trial Underway for Everolimus in Gastric Canceralmost 16 years ago
Soy foods may reduce recurrence risk in breast cancer patientsalmost 16 years ago
Genetic variations influence statin efficacy for lowering colon cancer riskalmost 16 years ago
Biomarkers signal true progress in war against lung canceralmost 16 years ago
Heart transplant patients face greater risk of skin canceralmost 16 years ago
Effective Rx for KRAS-mutated colon canceralmost 16 years ago
Pilot programs drive change in healthcare delivery modelNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.