Oncology NEWS International
- Oncology NEWS International Vol 15 No 4
- Volume 15
- Issue 4
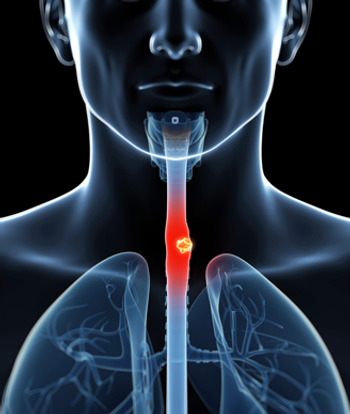
Trimodality Therapy Bests Surgery Alone for Resectable Esophageal Cancer Patients
Compared with surgery alone, the triple combination of chemotherapy, radiation therapy, and surgery is associated with a more than doubling of overall survival and a more than tripling of progression-free survival in patients with resectable esophageal cancer, according to a randomized trial presented at the 2006 Gastrointestinal Cancers Symposium (abstract 4).
SAN FRANCISCOCompared with surgery alone, the triple combination of chemotherapy, radiation therapy, and surgery is associated with a more than doubling of overall survival and a more than tripling of progression-free survival in patients with resectable esophageal cancer, according to a randomized trial presented at the 2006 Gastrointestinal Cancers Symposium (abstract 4).
"The concept behind this trial was to be a successor for the Intergroup study 0113. . . . That study looked at chemotherapy, followed by surgery and additional chemotherapy, compared with surgery alone," said lead author Mark J. Krasna, MD, chief of thoracic surgery, University of Maryland Medical Center. That study did not find a survival benefit for the combination therapy, he noted.
The new international and multi-institutional trial (CALGB 9781) randomized patients with stage I-III esophageal cancer to esophagectomy alone or to trimodality therapy consisting of combined chemotherapy (5-FU and cisplatin) and radiation therapy (50.4 Gy), followed 3 to 8 weeks later by esophagectomy.
Although target accrual was 400 patients, publication of favorable findings of another trial of trimodality therapy (N Engl J Med 335:462-467, 1996) led to reduced accrual. Final results were based on only 56 patients but were still dramatic enough to warrant reporting, he said. Patients were mostly male (91%) and white (86%); 75% had adenocarcinomas, typical of modern esophageal cancers in the United States.
At the time of surgery, Dr. Krasna said, the overall rate of pathologic response (complete response and partial response) in the trimodality group was 80%, while the rate of complete response alone was 40%. The preoperative therapy was associated with moderate morbidity: grade 3 hematologic toxicity in 54% of patients in this group, and grade 3 gastrointestinal toxicity (mainly esophagitis) in 40%.
Surgical complications occurred in 54% of patients in the surgery-alone arm and in 57% of those in the trimodality arm. There were two cases of leaks between the esophagus and stomach (both in the trimodality arm) and two cases of postoperative death (both in the surgery-alone arm). "The postoperative stay in the hospital was relatively short," Dr. Krasna noted (median 11.5 and 10 days in the surgery and trimodality groups, respectively). The median follow-up for the entire study population was 6 years.
Survival Differences 'Stark'
"The survival differences were stark," Dr. Krasna commented. Median overall survival in the trimodality group was more than double that in the surgery- alone group (4.5 vs 1.8 years). In addition, the 5-year survival rate differed significantly and was roughly three times higher in the former group than in the latter (39% vs 16%). Median progression-free survival also differed significantly between the trimodality and surgery groups (3.5 vs 1.0 years).
Patterns of failure were generally similar, although there tended to be more late distant recurrences and fewer early local ones with the combination than with surgery alone. In the trimodality arm, three patients had both local and distant recurrences, one had a local recurrence only, and five had a distant recurrence only. In the surgery-alone arm, one patient had both local and distant recurrences, three had a local recurrence only, and nine had a distant recurrence only.
"I think the important message that we can take from this trial is that there is actually a curative possibility for patients with esophageal cancer and that, hopefully, chemotherapy and radiation therapy followed by surgery will make a difference," he said. "Obviously, there are numerous treatment options for patients with esophageal cancer," with ongoing investigation of different variations on multimodality therapy.
Dr. Krasna noted that his institution is continuing to assess such therapy, with special attention to stage of disease. "I think that a possible stage-specific paradigm can be recommended: Surgery alone may be appropriate for very early stages of disease, such as a T1N0, whereas patients above this stage, T2s and T3s, and, of course, patients who are node positive, should be considered for chemotherapy and radiation therapy and surgery," he concluded.
Articles in this issue
almost 20 years ago
Phase II Trial of Velcade/Alimta Initiated in Advanced NSCLCalmost 20 years ago
ONS Annual Congress Heralds Start of Oncology Nursing Monthalmost 20 years ago
All-Star Panel Spells Out Onc Promises, Problemsalmost 20 years ago
Surveillance for Colon, Breast Ca Falls Off 5 Years After Diagnosisalmost 20 years ago
ODAC Says No to Gemzar for Ovarian Caalmost 20 years ago
Femara Effective Even After Years of No Therapyalmost 20 years ago
XMRV Retrovirus Found in Some Prostate Ca'salmost 20 years ago
Taxotere Wins FDA Approval for Advanced Gastric CancerNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.