Urine-Based DNA Test Can Help Diagnose Bladder Tumors
A novel urine-based DNA test was effective at detecting bladder cancer, and in particular at identifying patients with gross hematuria who do not require cystoscopy.
A novel urine-based DNA test was effective at detecting bladder cancer, and in particular at identifying patients with gross hematuria who do not require cystoscopy, according to a prospective, blinded study.
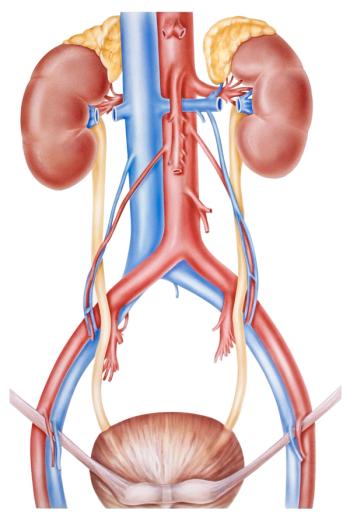
“Hematuria is the most common symptom of urothelial tumors in the urinary bladder, but is present in a host of other genitourinary conditions and is often idiopathic,” wrote study authors led by Per Guldberg, PhD, of the Danish Cancer Society Research Center in Copenhagen. Flexible cystoscopy, currently the standard for detecting bladder tumors, is invasive and does not have perfect accuracy. Retrospective studies have suggested that urine-based DNA testing could offer an alternative.
“A key component in our approach was a
Urine samples were tested for TERT and FGFR3 mutations, and methylation biomarkers (SALL3, ONECUT2, CCNA1, BCL2, EOMES, VIM).
On clinical examination, 99 patients (20.8%) were diagnosed with bladder cancer. Of those, a positive DNA test was obtained for one or both urine samples in 96 patients; a positive test was found in 87 out of the 376 patients without clinical evidence of malignancy.
These results yielded a sensitivity of 97%, and a specificity of 76.9%. It had a positive predictive value of 52.5%, and a negative predictive value of 99%. The test’s specificity was higher for samples obtained before cystoscopy (87.5% vs 81.7%; P = .04); sensitivity was not significantly different between the samples.
In all three cases where patients with evidence of cancer had negative DNA results, DNA obtained from the resected tumor was negative for all biomarkers. The authors wrote that this suggests “incomplete diagnostic coverage” of the biomarker panel. They also noted that long-term follow-up of patients with false positive results will help determine if these individuals are at increased risk of developing bladder cancer.
“With a negative predictive value for urothelial bladder tumor of 99%, urine-DNA testing may be used to identify a large subgroup of patients with gross hematuria in whom the cystoscopic component of the work-up is not required,” they concluded.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.