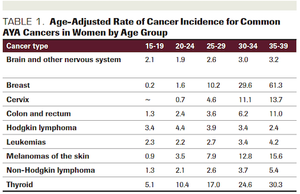
ABSTRACT Adolescents and young adults (AYAs) with cancer constitute approximately 70,000 patients diagnosed each year. Survival rates for AYAs with cancer have increased steadily in recent decades due to improvements in therapeutic regimens and early detection. Given the large and growing number of AYA cancer survivors, additional research is needed on the immediate and long-term psychosocial support required for this population including family planning and fertility. Fertility and fertility preservation in female AYAs, in particular, is historically understudied and has psychologically relevant ramifications distinct from male AYAs. Decision science can contribute to this area of oncological care and has implications for clinical encounters and research concerning female AYA patients with cancer. Patient-centered care and shared decision-making that integrates recent research regarding fertility preservation in the context of cancer treatment can improve outcomes for AYA cancer survivors.