Oncology NEWS International
- Oncology NEWS International Vol 11 No 7
- Volume 11
- Issue 7
Adding Monoclonal Antibody HuM195 Produces Higher Response Than Chemotherapy Alone in Advanced AML
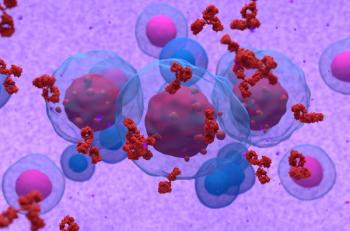
NEW YORK-Adding the monoclonal antibody HuM195 to chemotherapy for advanced acute myeloid leukemia (AML) produced a trend toward better patient response rates than chemotherapy alone in a phase III trial (ASCO abstract 1042).
NEW YORKAdding the monoclonal antibody HuM195 to chemotherapy for advanced acute myeloid leukemia (AML) produced a trend toward better patient response rates than chemotherapy alone in a phase III trial (ASCO abstract 1042).
Eric J. Feldman, MD, of the Weill Medical College of Cornell University in New York City said that the findings also suggest that the combination therapy might be more effective in certain subgroups of patients. "Our conclusion is that the drug has activity," Dr. Feldman told ONI. The results also support further testing at higher doses of HuM195, he added.
"In almost every category there is an improvement in response rate in patients receiving HuM195 over the control group," he said. This suggests, he noted, that these numbers might not have reached statistical significance because the study only randomized 191 patients and a low dose was used.
All Patients Received Standard Induction Therapy
HuM195 targets CD33, an antigen found on the majority of myeloid blasts. Previous trials had shown that it has modest anti-leukemic activity as a single agent, with responses primarily in AML patients with low-burden disease who had already been heavily treated.
The phase III study focused on hard-to-treat adult AML patients who did not respond initially to chemotherapy or who had their first remission within 1 year of treatment. Nearly two-thirds (64%) had had a complete response that lasted less than 6 months, and 26% had an antecedent blood disorder such as myelodysplastic syndrome.
All patients received standard induction therapy (mitoxantrone [Novantrone] at 8 mg/m² on days 1-6, etoposide at 80 mg/m² on days 1-6, and cytarabine 1 g/m² days on days 1-6). HuM195 was also administered to 94 patients as a 4-hour infusion on days 7 to 10 and days 19 to 22 at a dose of 12 mg/m². The remaining 97 patients did not receive any additional therapy.
Categories of Response
The patients who received the antibody-bolstered regimen had a higher overall response rate, 36% vs 28% of the patients who had chemotherapy alone. This included a higher rate of complete response (29% vs 23%) and more partial remissions (7% vs 5%).
Partial responders fell into a category the investigators called CRp and defined as having all the parameters of a complete response, but with a platelet count under 100,000. Dr. Feldman said patients in this category relapsed more quickly and had worse survival than complete responders.
"Most patients who achieved CRp were unable to undergo further chemotherapy, and only a very few had a bone marrow transplant option," he said, proposing that combination therapy might be less effective in patients who lack further treatment options, in particular, bone marrow transplantation.
Mortality rates during treatment were similar for the HuM195 and control arms: 15% and 13%, respectively. Patients ages 50 and under did substantially better than older patients, according to Dr. Feldman. Those who had gone 7 to 12 months before their cancer recurred also had better results than those with shorter time to remission.
HuM195 produced mild to moderate toxicity, primarily fever and chills during infusion. It did not increase chemotherapy-related toxicity, and the investigators concluded HuM195 could be safely combined with chemotherapy for patients with refractory AML.
Articles in this issue
over 23 years ago
Good Activity for Capecitabine Confirmed in European Studyover 23 years ago
Capecitabine/Vinorelbine Effective in Heavily Pretreated PatientsNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.