- ONCOLOGY Vol 13 No 9
- Volume 13
- Issue 9
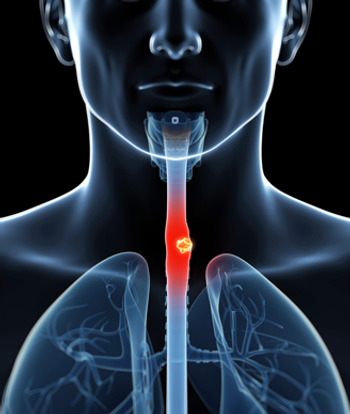
Carcinoma of the Esophagus Part 1: Primary Therapy
The two general treatment approaches for esophagel cancer include primary treatment (surgical or nonsurgical) or adjuvant treatment (preoperative or postoperative). Due to differences in the patient populations selected for
ABSTRACT: The two general treatment approaches for esophagel cancer include primary treatment (surgical or nonsurgical) or adjuvant treatment (preoperative or postoperative). Due to differences in the patient populations selected for surgical or nonsurgical therapies, which may bias the results against nonsurgical therapy, it is difficult to determine the best treatment approach for this disease. The standard of care is either surgery alone or primary combined-modality therapy. Based on a nonrandomized comparison of the data from recent intergroup trials, the results of these two approaches are similar. For patients treated without surgery, the intergroup INT 0123 trial will determine whether higher doses of radiation are of benefit. No clear survival advantage has been seen with preoperative or postoperative adjuvant radiation therapy alone or chemotherapy alone. The randomized trials comparing preoperative combined-modality therapy vs surgery alone reveal encouraging results for the combination appropach but need further confirmation. For patients treated with combined-modality therapy, the ideal regimen remains to be determined. The first part of this two-part article focuses on the rationale for and results of primary therapy for esophageal carcinoma. Part 2, which will appear in next months issue, covers adjunctive therapy. [ONCOLOGY 13(9):1225-1236,1999]
Two general approaches are used to treat esophageal cancer: primary treatment (surgical or nonsurgical) or adjuvant treatment (preoperative or postoperative). Primary treatments include surgery alone, radiation therapy alone, and radiation therapy plus chemotherapy (combined-modality therapy). Adjuvant therapies include preoperative or postoperative radiation therapy, preoperative chemotherapy, and preoperative combined-modality therapy. The first part of this two-part review will examine the rationale for and results of primary therapy for esophageal cancer. Part 2, which will appear in next months issue, deals with adjuvant therapy.
The epidemiology of esophageal cancer has changed during the past decade. The most notable change has been an increase in the incidence of adenocarcinoma, most commonly occurring at the gastroesophageal junction.[1] Therefore, histology should be considered when comparing the results of various treatment approaches. Adenocarcinoma is seen more frequently in middle-aged males with a history of gastroesophageal reflux, whereas squamous cell cancers occur more commonly in the proximal and middle esophagus of older patients who have a history of smoking and alcohol abuse.
At present, the available data are conflicting with respect to histology. Some series report different results according to histology, whereas other series report no such difference. Fortunately, the National Cancer Institutesponsored, intergroup, randomized trials are now stratified by histology. Until these stratified results are available, the impact of histology cannot be adequately assessed, and it is reasonable to treat both histologies in a similar fashion.
Surgical and nonsurgical approaches have had similar results when used as primary therapy for esophagel cancer. However, it must be emphasized that the patient population selected for treatment with each modality is usually different, resulting in a selection bias against nonsurgical therapy.
First, patients with poor prognostic features, including those who have medical contraindications to surgery and those with primary unresectable or metastatic disease, are more commonly selected for nonsurgical therapy. Second, surgical series report results based on pathologically staged patients, whereas nonsurgical series report results based on clinically staged patients. Pathologic staging has the advantage of excluding some patients with metastatic disease. Third, since some patients who receive nonsurgical therapy are treated palliatively rather than for cure, the intensity of chemotherapy and the doses and techniques of radiation therapy can be suboptimal.
Radiation Therapy Alone
Many series have reported the results of external-beam radiation therapy alone. Most of these series include patients with unfavorable features, such as clinical T4 disease and positive lymph nodes. For example, in the series by De-Ren, 184 of the 678 patients had stage IV disease.[2] Overall, the 5-year survival rate for patients treated with radiation therapy alone is 0% to 10%.[2-4]
The use of radiation therapy as a potentially curative modality requires doses of at least 5,000 cGy administered at 180 to 200 cGy per fraction. Furthermore, given the large size of many unresectable esophageal cancers, doses of ³ 6,000 cGy are probably required. However, even in the radiation therapy-alone arm of the Radiation Therapy Oncology Group (RTOG) trial 85-01, in which patients received 6,400 cGy of radiation delivered with modern techniques, all patients were dead from esophageal cancer by 3 years.[5,6]
There is one report of radiation therapy alone for patients with clinically early-stage disease. The trial by Sykes et al was limited to 101 patients (90% of whom had squamous cell carcinoma) with tumors < 5 cm who received 4,500 to 5,250 cGy in 15 to 16 fractions. The 5-year survival rate was 20%.[7]
In summary, radiation therapy alone should be reserved for palliation or for patients who are medically unable to receive chemotherapy. As will be discussed below, combined-modality therapy has had more favorable results and represents the standard of care.
Combined-Modality Therapy
Conventional ApproachesNumerous single-arm, nonrandomized trials have evaluated combined-modality therapy alone in patients with esophageal cancer.[8-12] Selected series are summarized in Table 1.
The series reported by Coia and associates is the only one in which patients with early-stage disease (clinical stages I and II) were analyzed separately from those with more advanced disease.[9] These patients were treated with flourouracil (5-FU) and mitomycin (Mutamycin) administered concurrently with 6,000 cGy of radiation. Combining clinical stages I and II, the local failure rate was 25%, the 5-year actuarial local relapse-free survival rate was 70%, and the 5-year actuarial survival rate was 30%.
The Southwest Oncology Group (SWOG) 9060 trial reported by Poplin et al included 32 patients who received 5-FU/cisplatin (Platinol) concurrently with 5,000 cGy of radiation, followed by two cycles of 5-FU/cisplatin.[13] Since the choice of further management (observation, radiation, chemotherapy, and/or surgery) was based on tumor response, this trial cannot be considered a pure combined-modality therapy series. Although the median survival was 20 months, the authors concluded that the complexity and toxicity of this combined-modality program precluded its further use.
Six randomized trials have compared radiation therapy alone with combined-modality therapy (Table 2).[5,14-19] Of the six trials, five used suboptimal doses of radiation and three employed inadequate doses of systemic chemotherapy.
For example, in the series by Araujo and colleagues,[14] patients received only one cycle of 5-FU, mitomycin, and bleomycin (Blenoxane). The European Organization for Research and Treatment of Cancer (EORTC) trial used subcutaneous methotrexate.[15] In the Scandinavian trial reported by Nygaard and associates, patients received low doses of chemotherapy (cisplatin [20 mg/m²] and bleomycin [10 mg/m²] for a maximum of two cycles).[16]
In the Eastern Cooperative Oncology Group (ECOG) EST-1282 trial, patients who received combined-modality therapy had significantly increased median survival, compared with those treated with radiation alone (15 vs 9 months; P = .04), but showed no improvement in 5-year survival (9% vs 7%). However, this was not a pure nonsurgical trial since approximately 50% of patients in each arm underwent surgery after receiving 4,000 cGy of radiation. Furthermore, this decision depended on the individual investigators preference. Operative mortality was 17%.
Lastly, the Pretoria trial reported by Slabber and colleagues, which was limited to a total of 70 patients with T3 squamous cell cancers, used a low-dose (4,000-cGy) split-course radiation schedule.[18]
The only trial designed to deliver adequate doses of systemic chemotherapy with concurrent radiation therapy was the RTOG 85-01 trial reported by Herskovic et al (Figure 1).[5,17] This intergroup trial primarily included patients with squamous cell carcinoma. They received four cycles of 5-FU (1,000 mg/m²/24 h × 4 days) and cisplatin (75 mg/m² on day 1). Radiation therapy (5,000 cGy at 200-cGy/d) was given concurrently with day 1 of chemotherapy. Curiously, cycles 3 and 4 of chemotherapy were delivered every 3 weeks (weeks 8 and 11) rather than every 4 weeks (weeks 9 and 13). This intensification may explain, in part, why only 50% of the patients finished all four cycles of chemotherapy. The control group received radiation therapy alone, albeit at a higher dose (6,400 cGy) than patients in the combined-modality therapy arm.
Patients who received combined-modality therapy demonstrated a significant improvement in median survival (14 vs 9 months) and 5-year survival (27% vs 0%; P < .0001), compared with radiation alone.[17] The actuarial incidence of local failure as the first site of failure was also significantly decreased in the combined-modality group (45% vs 68%; P = .0123).
The protocol was closed early due to these positive results. Following this early closure, an additional 69 patients were treated with the same combined-modality therapy regimen, and similar results were seen (3-year survival rate of 30%).
ToxicityAlthough combined-modality therapy achieves better results than radiation alone, it is associated with a higher incidence of toxicity. In the RTOG 85-01 trial, patients who received combined-modality therapy had more acute grade 3 toxicity (44% vs 25%) and acute grade 4 toxicity (20% vs 3%) than patients given radiation therapy alone. Including the one treatment-related death (2%), the total incidence of acute grade 3+ toxicity in this trial was 66%. Although the acute grade 3+ radiation-related toxicity was higher with combined-modality therapy than with radiation therapy alone (35% vs 12%), there was little difference in late toxicity (29% vs 23%).
Based on the positive results of the RTOG 85-01 trial, the conventional nonsurgical treatment for esophageal carcinoma is combined-modality therapy. These results notwithstanding, the local failure rate in the RTOG 85-01 combined-modality therapy arm was 45%. Thus, there is room for improvement, and new approaches, such as intensification of combined-modality therapy and escalation of the radiation dose, have been developed in an attempt to improve upon these results.
Intensification of Combined-Modality TherapyThe phase II intergroup INT 0122 trial [ECOG PE289/RTOG 9012] was designed to intensify the RTOG 85-01 combined-modality arm.[20 ] The development of the neoadjuvant chemotherapy approach used in INT 0122 was based, in part, on the results of a randomized trial of preoperative radiation therapy (5,500 cGy) vs preoperative chemotherapy (5-FU/cisplatin/vindesine [Eldisine]) from Memorial Sloan-Kettering Cancer Center. That trial revealed similar results with preoperative radiation therapy and preoperative chemotherapy with regard to resectability (65% vs 58%), objective responses (64% vs 55%), and local failure rates (15% vs 6%).[21]
As seen in Figure 2, both the chemotherapy and radiation therapy regimens in INT 0122 were intensified as follows: (1) The continuous infusion of 5-FU (1,000 mg/m²/24 h) was increased from 4 to 5 days. (2) The total number of cycles of chemotherapy was increased from four to five.(3) Three cycles of full-dose neoadjuvant 5-FU/cisplatin were delivered prior to the start of combined-modality therapy. (4) The radiation dose was increased from 5,000 to 6,480 cGy. Eligibility was limited to patients with squamous cell carcinoma; 45 patients were entered into the trial, 38 of whom were eligible.
The final results of the intergroup (INT) 0122 trial were reported recently.[20] Of the 38 eligible patients, 47% had complete primary tumor responses; 8%, partial responses; and 3%, stable disease. The first site of clinical failure was local in 39% of patients and distant in 24%. For the total patient group, there were 6 deaths during treatment, of which 9% (4/45) were treatment-related. The median survival time was 20 months, and the 5-year actuarial survival rate was 20%.
Therefore, this intensive, neoadjuvant approach did not appear to offer a benefit compared with conventional doses and techniques of combined-modality therapy. However, the higher radiation dose (6,480 cGy) was tolerable and is being tested further in INT 0123, which is the follow-up trial to RTOG 85-01 (Figure 3).
Neoadjuvant Chemotherapy Prior to Radiation or Combined-Modality TherapyA limited number of phase II trials have tested the use of neoadjuvant chemotherapy prior to radiation therapy or combined-modality therapy. Valerdi et al reported the results of 40 patients with clinical stage II and III squamous cell cancers who received two cycles of neoadjuvant cisplatin/vindesine/bleomycin (on days 1 and 29), followed by 6,000 cGy of radiation.[12] In contrast to INT 0122, no chemotherapy was delivered with the radiation therapy in this trial.
The pathologic complete response rate was 53%. With a median follow-up of 78 months, the local failure rate was 62%, median survival duration was 11 months, and the 5-year actuarial survival rate was 15%. These results are similar to those obtained with the RTOG 85-01 combined-modality arm, with the exception of a higher treatment-related death rate (5%).
Using a five-drug neoadjuvant regimen, Roca and colleagues treated 55 patients (54 with squamous cell carcinoma) with bolus cisplatin/5-FU/leucovorin/bleomycin/mitomycin for 15 days, followed by 6,000 cGy of radiation plus concurrent 5-FU/leucovorin/cisplatin.[22] No maintenance chemotherapy was delivered. Patients with disease at all anatomic sites within the esophagus were eligible, and 53% had clinical stage III disease. Although treatment-related mortality was only 4% and the 3-year survival rate was 35%, the local failure rate (as a component of failure) was 42%, which was similar to the 45% rate reported in the RTOG 85-01 combined-modality therapy arm.
In summary, neoadjuvant chemotherapy, as delivered in the trials described above, does not appear to improve on the results of combined-modality therapy. New trials using paclitaxel (Taxol)-based neoadjuvant chemotherapy are in progress.[23]
Intensification of the Radiation DoseAnother approach to the dose intensification of combined-modality therapy is to increase the radiation dose above 6,000 cGy. Two methods are used to increase the radiation dose to the esophagus: brachytherapy and external-beam therapy.
BrachytherapyIntraluminal brachytherapy allows the escalation of the dose to the primary tumor while protecting the surrounding dose-limiting structures, such as the lung, heart, and spinal cord.[24] A radioactive source is placed intraluminally via bronchoscopy or a nasogastric tube.
Brachytherapy has been used both as a primary therapy[25] and as a boost following external-beam radiation therapy.[26,27] It can be delivered by high dose rate or low dose rate.[28] Although there are technical and radiobiological differences between the two dose rates, neither has shown a clear therapeutic advantage.
As a primary therapy, brachytherapy results in a local control rate of 25% to 35%.[26,29] A randomized trial conducted by Sur et al found no significant difference in local control or survival with high-dose-rate brachytherapy compared with external-beam therapy.[29]
A major limitation of brachytherapy is the effective treatment distance. The primary isotope is iridium-192, which is usually prescribed so as to treat to a distance of 1 cm from the source. Therefore, any portion of the tumor that is > 1 cm from the source will receive a suboptimal radiation dose.
A phase II trial by Calais et al reported encouraging results with intraluminal brachytherapy.[27] A total of 53 patients with clinically unresectable adenocarcinoma or squamous cell carcinoma of the esophagus received 6,000 cGy of external-beam radiation plus three cycles of concurrent 5-FU/cisplatin/mitomycin, followed by high-dose-rate intraluminal brachytherapy (500 cGy/wk × 2) prescribed to 0.5 cm. With a median follow-up of 39 months, the 3-year and 5-year actuarial survival rates were 27% and 18%, respectively.
Severe late toxicity occurred in 11% of patients. One patient died of treatment-related toxicity. Although two patients (4%) developed a fistula, both were due to tumor progression. Swallowing function was good in 75% of patients. The local failure rate was 43% (23/53).
These results are comparable to those of other trials of combined-modality therapy. Therefore, the benefit of adding intraluminal brachytherapy is unclear.
In the RTOG 92-07 trial, 75 patients with squamous cell cancers (92%) or adenocarcinomas (8%) of the thoracic esophagus received the RTOG 85-01 combined-modality regimen (5-FU/cisplatin × 4 with concurrent radiation [5,000 cGy]), followed, during cycle 3 of chemotherapy, by a boost with either low-dose-rate (19 patients) or high-dose-rate (56 patients) intraluminal brachytherapy.[30] The choice of the dose rate was at the discretion of the investigator.
Due to low patient accrual, the low-dose-rate option was discontinued, and the analysis was limited to patients who received the high-dose-rate treatment. High-dose-rate brachytherapy was delivered in weekly fractions of 500 cGy during weeks 8, 9, and 10. Following the development of several fistulas, the fraction delivered at week 10 was discontinued.
Although the complete response rate was 73%, with a median follow-up of only 11 months, the rate of local failure as the first site of failure was 27%. Acute toxicity included a 58% incidence of grade 3 events, a 26% rate of grade 4 toxicity, and a 8% of grade 5 events (treatment-related death). The cumulative incidence of fistula was 18% per year and the crude incidence was 14%. Of the six treatment-related fistulas, three were fatal. Given the significant toxicity, this treatment approach should be used with caution.
The American Brachytherapy Society has developed guidelines for esophageal brachytherapy.[31] For patients treated in the curative setting, brachytherapy should be limited to tumors £ 10 cm with no evidence of distant metastasis. Contraindications to brachytherapy include tracheal or bronchial involvement, cervical esophagus location, or stenosis that cannot be bypassed. The applicator should have an external diameter of 6 to 10 cm.
If combined-modality therapy (defined as 5-FUbased chemotherapy plus 4,500 to 5,000 cGy of radiation) is used, the recommended doses of brachytherapy are: high dose rate, 1,000 cGy in 2 weekly fractions of 500 cGy each; or low-dose rate, 2,000 cGy in a single fraction at 40 to 100 cGy/h. The doses should be prescribed to 1 cm from the mid-source. Lastly, brachytherapy should be delivered after the completion of external-beam therapy and not concurrently with chemotherapy.
External-Beam TherapyThere are limited data on the tolerance of patients to external-beam doses of ³ 6,000 cGy when delivered concurrently with chemotherapy. A separate toxicity analysis by Coia and associates, which included 90 patients with clinical stages I-IV squamous and adenocarcinomas of the esophagus, reported a 22% incidence of grade 3 toxicity and a 6% rate of grade 4 toxicity.[9] There were no treatment-related deaths.
Calais et al pubished the results of 53 patients with clinically unresectable disease who received 5-FU/cisplatin/mitomycin plus 6,500 cGy of radiation.[32] The full dose of radiation could be delivered in 96% of patients. The incidence of World Health Organization (WHO) grade 3+ toxicity was 30%, and the overall 2-year survival rate was 42%. It should be noted that the chemotherapy used in this trial was not delivered at doses adequate to treat systemic disease.
On an encouraging note, almost all patients in both INT 0122 and the trial by Calais et al (96% and 94%, respectively) who started radiation therapy were able to receive the full dose (6,480 to 6,500 cGy). Therefore, this higher radiation dose was considered to be tolerable and is being used in the experimental arm of the intergroup esophageal trial INT 0123 (RTOG 9405). As mentioned above, INT 0123 is the follow-up trial to RTOG 8501. In this trial, patients with either squamous cell or adenocarcinomas who are selected for a nonsurgical approach are being randomized to a slightly modified RTOG 85-01 combined-modality regimen plus 5,040 cGy of radiation vs the same chemotherapy plus 6,480 cGy (Figure 3).
The modifications to the original RTOG 85-01 combined-modality therapy arm include: (1) using 180-cGy fractions to 5,040 cGy rather than 200-cGy fractions to 5,000 cGy; (2) treating the tumor plus 5-cm proximal and distal margins for 5,040 cGy rather than treating the whole esophagus for the first 3,000 cGy followed by a boost to the primary tumor with 5 cm proximal and distal margins to 5,000 cGy; (3) delaying cycle 3 of 5-FU/cisplatin until 4 weeks following the completion of radiation therapy rather than until 3 weeks post-radiation; and (4) delivering cycles 3 and 4 of chemotherapy every 4 weeks rather than every 3 weeks. The INT 0123 opened in late 1994.
In addition to increasing the total dose, radiation can be intensified by accelerated fractionation or hyperfractionation. Selected series using this approach are shown in Table 3.[33-35] Although these approaches are reasonable, most series report an increase in acute toxicity without any clear therapeutic benefit. Therefore, these regimens remain investigational.
Dysphagia is a common problem in patients with esophageal cancer. Not only is it the most frequently presenting symptom, but also it can remain a problem up to the time of the patients death.
Major weaknesses of the series examining palliation are that they are retrospective and most do not use objective criteria to define and assess dysphagia. Some studies do not report the number of patients presenting with dysphagia or the percentage who are palliated until the time of death. Furthermore, few series carefully examine other variables that may influence the results, such as histology, stage, and location of the primary tumor.
As seen in Table 4, a limited number of series have examined the palliative benefits of either radiation therapy alone[15,36-39] or combined-modality therapy.[10,11,38,40-42] Overall, external radiation therapy alone palliates dysphagia in approximately 70% to 80% of patients.
The most comprehensive, carefully performed analysis of swallowing function in patients receiving combined-modality therapy was conducted by Coia and colleagues.[43] Using a swallowing score modified from ORourke et al,[44] Coia et al analyzed 102 patients treated with three 5-FUbased combined-modality regimens. Prior to the start of therapy, 95% of patients had some degree of dysphagia.
Within 2 weeks following the start of treatment, 45% of patients experienced an improvement in dysphagia, and by the completion of the 6 weeks of therapy, this percentage had increased to 83%. Overall, dysphagia improved in 88% of patients. The median time to maximum improvement was 4 weeks (range, 1 to 21 weeks), and all but two patients could swallow at least soft or solid foods at the time of maximum symptomatic improvement.
This study also examined such variables as intent of treatment, histology, stage, and tumor location. In the 25 patients treated with curative intent who survived more than 1 year, all were able to eat soft or solid foods following treatment. The benign stricture rate (defined as a stricture in the absence of recurrent disease) was 12%. Even in patients who were not treated with curative intent, 91% experienced an initial improvement in swallowing, and 67% were palliated until the time of their death.
Histology and stage had no impact of the rate of palliation. However, dysphagia improved in significantly more patients with a lesion in the distal third of the esophagus than in those with a tumor in the upper two-thirds (95% vs 79%; P < .05).
Intraluminal brachytherapy also is an effective, albeit more limited, palliative method. It achieves palliation of dysphagia in 40% to 90% of patients.[26,29] As previously discussed, since brachytherapy is usually prescribed to 1 cm from the source, it may underdose gross disease.
There is a selection bias against brachytherapy since it is commonly used for patients who have either not responded to external-beam therapy or who are medically unable to travel for daily outpatient treatment. Even accounting for these selection biases, given its limited effective range, intraluminal brachytherapy is usually not as successful as external-beam radiation in treating the entire tumor volume.
In summary, external-beam radiation therapy, either alone or in combination with chemotherapy, relieves dysphagia in approximately 80% of patients, half of whom are palliated until the time of their death. If a patient requires rapid palliation (within a few days), alternative approaches, such as laser therapy or stenting, are recommended.
Although external-beam radiation, with or without chemotherapy, requires at least 2 weeks to relieve dysphagia, once palliation is achieved, it is more durable than that is produced by other palliative modalities since radiation treats the problem (the gross tumor mass), not just the symptom. If external-beam radiation cannot be used, brachytherapy should be considered.
The toxicity of radiation therapy is a function of the total radiation dose and technique used and whether the patient has received chemotherapy. There are limited toxicity data on patients who have received conventional doses of radiation therapy.
The most carefully documented data on acute radiation-related toxicity come from the control arm of RTOG 85-01, in which patients received radiation therapy alone to a dose of 6,400 cGy.[5,17] The incidence of acute grade 3 toxicity was 25% and the rate of grade 4 toxicity was 3%. No treatment-related deaths occurred.
Like surgery, radiation therapy can produce esophageal strictures. The total incidence of strictures (benign plus malignant) in patients receiving radiation therapy alone or combined with chemotherapy is 20% to 40% in modern series and up to 60% in historical series.[45]
It should be noted that almost half of these strictures are malignant since they are associated with a local recurrence. Furthermore, the incidence of stricture is lower in series in which careful radiation techniques were used. For example, Coia et al examined a subset of 25 patients whose disease was controlled locally and who survived for at least 1 year. The incidence of benign strictures in this study was 12%.[43]
One study examined the functional results in patients who developed benign or malignant strictures.[44] In this study, 80 patients received 4,500 to 5,600 cGy of radiation and 53% received some form of chemotherapy. Of the 24 patients (30%) who developed a benign stricture, 71% were able to tolerate a full or soft diet and required dilation (median interval between dilations, 5 months). Therefore, even in this subset of patients who developed a benign stricture, dilation was effective in the majority of patients. In contrast, in the 28% of patients who developed a malignant stricture, dilation was unsuccessful and esophageal intubation was required.
The high incidence of fistulas reported in the RTOG 92-07 trial of combined-modality therapy plus intraluminal brachytherapy (18% actuarial, 14% crude) has not been reported in series using radiation therapy or combined-modality therapy without intraluminal brachytherapy. The incidence of other long-term grade 3+ toxicities, such as pneumonitis and pericarditis, is 5%. If appropriate radiation doses and techniques are used, spinal cord myelitis should not occur.
The issue of treatment-related deaths in patients receiving combined-modality therapy in intergroup trials is complex. Although treatment-related mortality was only 2% in RTOG 85-01, subsequent trials have reported higher treatment-related death rates (ie, 9% in INT 0122 and 8% in RTOG 9207). These death rates are lower than the 10% to 15% incidence reported in the historical surgical series, although they are only slightly higher than the 6% rate reported in the surgical control arm of INT 0113.
It is interesting to note that as mortality associated with surgery has decreased, there has been a corresponding increase in treatment-related mortality reported in trials of nonoperative therapies. As previously discussed, this may be related, in part, to improved surgical techniques or possible selection bias against patients treated with the nonoperative approach. Only a randomized trial of surgical vs nonsurgical therapy can address this issue.
Similar to the studies of radiation therapy alone, most of the results reported with surgery alone derive from historical series. These trials report 5-year survival rates of 5% to 20%. The results of the surgical control arms from two recently published randomized trials of preoperative chemotherapy in patients with clinically resectable disease offer a more accurate assessment of results. In these trials, patients underwent an Ivor-Lewis esophagectomy or a transhiatal procedure.
In the Dutch trial of preoperative chemotherapy reported by Kok et al, the 160 patients in the surgical control arm had a median survival time of 11 months.[46] Similar results were reported in the 234 patients (110 with squamous cell carcinoma and 124 with adenocarcinoma) in the surgical control arm of the INT 0113 (RTOG 89-11) trial.[47] Operative mortality was 6%. With a median follow-up of 55 months, the median survival duration was 16 months, the 5-year survival rate was 20%, and the incidence of local failure as the first site of failure in the 59% of patients who underwent a complete resection with negative margins (R0 resection) was 31%.
Some surgeons, primarily based in Japan, advocate a three-field dissection rather than a more conventional Ivor-Lewis or transhiatal esophagectomy. With this unusually aggressive surgical approach, regardless of the location of the primary tumor, patients undergo dissection of the lymph nodes in the neck, mediastinum, and celiac axis.
In a report by Bhansali et al of 90 patients with squamous cell cancers (57% of whom received preoperative chemotherapy or radiation therapy), the 5-year survival rate was 39%.[48] However, the local failure rate was still 72%, and there was a high incidence of postoperative complications (ie, a 74% rate of recurrent laryngeal nerve paralysis, 32% incidence of anastomotic leak, and 26% rate of aspiration pneumonia). Nishimaki et al reported a morbidity of 58% in 190 patients treated with this technique.[49]
In summary, most investigators outside of Japan do not advocate this more aggressive surgical approach.
Due to the selection bias that results in patients who have clinically resectable disease and are medically fit being chosen for surgery, it is difficult to compare the results of nonsurgical and surgical approaches in the absence of a randomized trial. Despite the adverse selection factors, a comparison of the results of these respective treatment approaches from the national intergroup trials reveals that the nonsurgical approaches offer a survival rate that is the same as if not better than surgery, as well as improved palliation of dysphagia.
For example, median survival and the 5-year survival rate were 14 months and 27%, respectively, in the combined-modality therapy arm of RTOG 85-01 and 20 months and 20%, respectively, in INT 0122. In comparison, the median survival in the surgical control arm of the Dutch trial by Kok et al was 11 months and median survival and the 5-year survival rate in the surgical control arm of INT 0113 were 16 months and 20%, respectively.
Likewise, the local failure rates were similar. The rates of local failure (local failure plus local persistence of disease) as the first site of failure were 45% in RTOG 85-01 and 39% in INT 0122. Although the incidence of local failure as the first site of failure in INT 0113 was 31%, it must be emphasized that this analysis was limited to patients who underwent a complete resection with negative margins (R0 resection). Since an additional 30% of patients had residual local disease, if one was to score these patients as having local persistent disease (as was done in the RTOG 85-01 analysis), the comparable local failure rate with surgery alone was 30% plus 31%, or 61%. The treatment-related death rates were also similar (2% in RTOG 85-01, 9% in INT 0122, and 6% in INT 0113).
In summary, the local failure, survival, and treatment-related death rates of nonsurgical and surgical therapies are similar. Although the results are comparable, it is clear that both the nonsurgical and surgical approaches have limited success. Therefore, trials that have combined the two approaches (surgery plus preoperative or postoperative adjuvant therapy) have been developed. These adjuvant approaches will be discussed next month in part 2 of this article.
References:
1. Phillips TL, Minsky BD, Dicker A, et al: Cancer of the esophagus, in Leibel SA and Phillips TA (eds): Textbook of Radiation Oncology, pp 601-623. Philadelphia, WB Saunders, 1998.
2. De-Ren S: Ten-year follow-up of esophageal cancer treated by radical radiation therapy: Analysis of 869 patients. Int J Radiat Oncol Biol Phys 16:329-334, 1989.
3. Newaishy GA, Read GA, Duncan W, et al: Results of radical radiotherapy of squamous cell carcinoma of the esophagus. Clin Radiol 33:347-352, 1982.
4. Okawa T, Kita M, Tanaka M, et al: Results of radiotherapy for inoperable locally advanced esophageal cancer. Int J Radiat Oncol Biol Phys 17:49-54, 1989.
5. Herskovic A, Martz LK, Al-Sarraf M, et al: Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus. N Engl J Med 326:1593-1598, 1992.
6. Al-Sarraf M, Martz K, Herskovic A, et al: Superiority of chemo-radiotherapy (CT-RT) vs radiotherapy (RT) in patients with esophageal cancer: Final report of an intergroup randomized and confirmed study (abstract). Proc Am Soc Clin Oncol 15:206, 1996.
7. Sykes AJ, Burt PA, Slevin NJ, et al: Radical radiotherapy for carcinoma of the oesophagus: An effective alternative to surgery. Radiother Oncol 48:15-21, 1998.
8. John MJ, Flam M, Ager Mowry PA, et al: Radiotherapy alone and chemoradiation for nonmetastatic esophageal carcinoma. Cancer 63:2397-2403, 1989.
9. Coia LR, Engstrom PF, Paul AR, et al: Long-term results of infusional 5-FU, mitomycin-C, and radiation as primary management of esophageal cancer. Int J Radiat Oncol Biol Phys 20:29-36, 1991.
10. Izquierdo MA, Marcuello E, Gomez de Segura G, et al: Unresectable nonmetastatic squamous cell carcinoma of the esophagus managed by sequential chemotherapy (cisplatin and bleomycin) and radiation therapy. Cancer 71:287-292, 1993.
11. Seitz JF, Giovannini M, Padaut-Cesana J, et al: Inoperable nonmetastatic squamous cell carcinoma of the esophagus managed by concomitant chemotherapy (5-fluorouracil and cisplatin) and radiation therapy. Cancer 66:214-219, 1990.
12. Valerdi JJ, Tejedor M, Illarramendi JJ, et al: Neoadjuvant chemotherapy and radiotherapy in locally advanced esophagus carcinoma: Long-term results. Int J Radiat Oncol Biol Phys 27:843-847, 1994.
13. Poplin EA, Jacobson J, Herskovic A, et al: Evaluation of multimodality treatment of locoregional esophageal carcinoma by Southwest Oncology Group 9060. Cancer 78:1851-1866, 1996.
14. Araujo CMM, Souhami L, Gil RA, et al: A randomized trial comparing radiation therapy vs concomitant radiation therapy and chemotherapy in carcinoma of the thoracic esophagus. Cancer 67:2258-2261, 1991.
15. Roussel A, Jacob JH, Jung GM, et al: Controlled clinical trial for the treatment of patients with inoperable esophageal carcinoma: A study of the EORTC gastrointestinal tract cancer cooperative group, in Schlag P, Hohenberger P, Metzger U (eds): Recent Results in Cancer Research, 1st ed, pp 21-30. Berlin, Springer-Verlag, 1988.
16. Nygaard K, Hagen S, Hansen HS, et al: Pre-operative radiotherapy prolongs survival in operable esophageal carcinoma: A randomized, multicenter study of pre-operative radiotherapy and chemotherapy: The second Scandinavian trial in esophageal cancer. World J Surg 16:1104-1110, 1992.
17. Al-Sarraf M, Martz K, Herskovic A, et al: Progress report of combined chemoradiotherapy vs radiotherapy alone in patients with esophageal cancer: An intergroup study. J Clin Oncol 15:277-284, 1997.
18. Slabber CF, Nel JS, Schoeman L, et al: A randomized study of radiotherapy alone vs radiotherapy plus 5-fluorouracil and platinum in patients with inoperable, locally advanced squamous cell cancer of the esophagus. Am J Clin Oncol (CCT) 21:462-465, 1998.
19. Smith TJ, Ryan LM, Douglass HO, et al: Combined chemoradiotherapy vs radiotherapy alone for early stage squamous cell carcinoma of the esophagus: A study of the Eastern Cooperative Oncology Group. Int J Radiat Oncol Biol Phys 42:269-276, 1998.
20. Minsky BD, Neuberg D, Kelsen DP, et al: Final report of intergroup trial 0122 (ECOG PE-289, RTOG 90-12): Phase II trial of neoadjuvant chemotherapy plus concurrent chemotherapy and high-dose radiation for squamous cell carcinoma of the esophagus. Int J Radiat Oncol Biol Phys 43:517-523, 1999.
21. Kelsen DP, Minsky BD, Smith M, et al: Preoperative therapy for esophageal cancer: A randomized comparison of chemotherapy vs radiation therapy. J Clin Oncol 8:1352-1361, 1990.
22. Roca E, Pennella E, Sardi M, et al: Combined intensive chemoradiotherapy for organ preservation in patients with resectable and nonresectable oesophageal cancer. Eur J Cancer 32A:429-432, 1996.
23. Kelsen D, Ilson D, Lipton R, et al: A phase I trial of radiation therapy (RT) plus concurrent fixed dose cisplatin (C) with escalating doses of paclitaxel (P) as a 96-hour continuous infusion in patients (PTS) with localized esophageal cancer (EC) (abstract). Proc Am Soc Clin Oncol 18:271, 1999.
24. Armstrong JG. High-dose rate remote afterloading brachytherapy for lung and esophageal cancer. Semin Radiat Oncol 4:270-277, 1993.
25. Jager J, Langendijk H, Pannebakker M, et al: A single session of intraluminal brachytherapy in palliation of esophageal cancer. Radiother Oncol 37:237-240, 1995.
26. Moni J, Armstrong JG, Minsky BD, et al: High-dose rate intraluminal brachytherapy for carcinoma of the esophagus. Dis Esophagus 9:123-127, 1996.
27. Calais G, Dorval E, Louisot P, et al: Radiotherapy with high-dose rate brachytherapy boost and concomitant chemotherapy for stages IIB and III esophageal carcinoma: Results of a pilot study. Int J Radiat Oncol Biol Phys 38:769-775, 1997.
28. Caspers RJL, Zwinderman AH, Griffioen G, et al: Combined external beam and low-dose rate intraluminal radiotherapy in oesophageal cancer. Radiother Oncol 27:7-12, 1993.
29. Sur RK, Singh DP, Sharma SC: Radiation therapy of esophageal cancer: role of high-dose rate brachytherapy. Int J Radiat Oncol Biol Phys 22:1043-1046, 1992.
30. Gaspar LE, Qian C, Kocha WI, et al: A phase I/II study of external beam radiation, brachytherapy, and concurrent chemotherapy in localized cancer of the esophagus (RTOG 92-07): Preliminary toxicity report. Int J Radiat Oncol Biol Phys 37:593-599, 1997.
31. Gaspar LE, Nag S, Herskovic A, et al: American Brachytherapy Society (ABS) consensus guidelines for brachytherapy of esophageal cancer. Int J Radiat Oncol Biol Phys 38:127-132, 1997.
32. Calais G, Jadaud E, Chapet S, et al: High dose radiotherapy (RT) and concomitant chemotherapy for nonresectable esophageal cancer: Results of a phase II study (abstract). Proc Am Soc Clin Oncol 13:197, 1994.
33. Girinsky T, Auperin A, Marsiglia H, et al: Accelerated fractionation in esophageal cancers: A multivariate analysis on 88 patients. Int J Radiat Oncol Biol Phys 38:1013-1018, 1997.
34. Powell MEB, Hoskin PJ, Saunders MT, et al: Continuous hyperfractionated accelerated radiotherapy (CHART) in localized cancer of the esophagus. Int J Radiat Oncol Biol Phys 38:133-136, 1997.
35. Jeremic B, Shibamoto Y, Acimovic L, et al: Accelerated hyperfractionated radiation therapy and concurrent 5-fluorouracil/cisplatin chemotherapy for locoregional squamous cell carcinoma of the thoracic esophagus: A phase II study. Int J Radiat Oncol Biol Phys 40:1061-1066, 1998.
36. Wara WM, Mauch PM, Thomas AN, et al: Palliation for carcinoma of the esophagus. Radiology 121:717-720, 1976.
37. Petrovich Z, Langholz B, Formenti S, et al: Management of carcinoma of the esophagus: The role of radiotherapy. Am J Clin Oncol (CCT) 14:80-86, 1991.
38. Whittington R, Coia LR, Haller DG, et al: Adenocarcinoma of the esophagus and esophagogastric junction: The effects of single and combined modalities on the survival and patterns of failure following treatment. Int J Radiat Oncol Biol Phys 19:593-603, 1990.
39. Caspers RJL, Welvaart K, Verkes RJ, et al: The effect of radiotherapy on dysphagia and survival in patients with esophageal cancer. Radiother Oncol 12:15-23, 1988.
40. Algan O, Coia LR, Keller SM, et al: Management of adenocarcinoma of the esophagus with chemoradiation alone or chemoradiation followed by esophagectomy: Results of sequential nonrandomized phase II studies. Int J Radiat Oncol Biol Phys 32:753-761, 1995.
41. Gill PG, Denham JW, Jamieson GG, et al: Patterns of treatment failure and prognostic factors associated with the treatment of esophageal carcinoma with chemotherapy and radiotherapy either as sole treatment of followed by surgery. J Clin Oncol 10:1037-1043, 1992.
42. Urba SG, Turrisi AT: Split-course accelerated radiation therapy combined with carboplatin and 5-fluorouracil for palliation of metastatic or unresectable carcinoma of the esophagus. Cancer 75:435-439, 1995.
43. Coia LR, Soffen EM, Schultheiss TE, et al: Swallowing function in patients with esophageal cancer treated with concurrent radiation and chemotherapy. Cancer 71:281-286, 1993.
44. ORourke IC, Tiver K, Bull C, et al: Swallowing performance after radiation therapy for carcinoma of the esophagus. Cancer 61:2022-2026, 1988.
45. Minsky BD: Radiation therapy in the treatment of esophagus cancer. Chest Surg Clin North Am 4:285-297, 1994.
46. Kok TC, Lanschot JV, Siersema PD, et al: Neoadjuvant chemotherapy in operable esophageal squamous cell cancer: Final report of a phase III multicenter randomized trial (abstract). Proc Am Soc Clin Oncol 16:277, 1997.
47. Kelsen DP, Ginsberg R, Pajak T, et al: Chemotherapy followed by surgery compared with surgery alone for localized esophageal cancer. N Engl J Med 339:1979-1984, 1998.
48. Bhansali MS, Fujita H, Kakegawa T, et al: Pattern of recurrence after extended radical esophagectomy with three-field lymph node dissection for squamous cell carcinoma in the thoracic esophagus. World J Surg 21:275-281, 1997.
49. Nishimaki T, Suzuki T, Suzuki S, et al: Outcomes of extended radical esophagectomy for thoracic esophageal cancer. J Am Coll Surg 186:306-312, 1998.
Articles in this issue
over 26 years ago
Lowering Drug Prices for Non-Medicare Patientsover 26 years ago
Paclitaxel Improves Survival in Metastatic Breast Cancerover 26 years ago
FDA Plans Crackdown on Online Drug Salesover 26 years ago
p53 Gene Therapy Shows Activity Against Head and Neck Cancerover 26 years ago
OTC Analgesic Gel Treats Oral Ulcers in Chemotherapy Patientsover 26 years ago
September Is Gynecologic Cancer Awareness Monthover 26 years ago
Improving the Chemotherapy Experienceover 26 years ago
Chemoradiation an Effective But Toxic Therapy for Colorectal Cancerover 26 years ago
Oncologists Likely to Get Small Medicare Increasesover 26 years ago
Global Progress: Breast Cancer MortalityNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.