Chemoradiotherapy De-escalation Appears Feasible in HPV+ Oropharynx Cancer
The role of multimodal approaches such as FDG-PET imaging may require further investigation in patients with human papillomavirus–positive oropharyngeal cancer, according to Samuel Regan, MD.
“We plan to continue to investigate the role of multimodal approaches for de-escalation of therapy for this patient population,” according to Samuel Regan, MD.
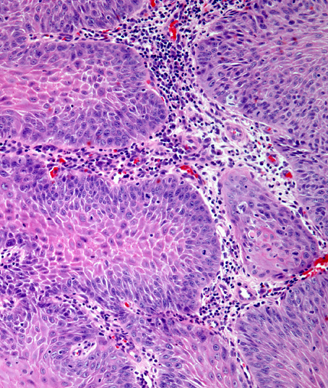
Deescalating chemoradiotherapy (CRT) based on FDG-PET appeared feasible and yielded few regional recurrences in patients with human papillomavirus (HPV)–positive oropharyngeal squamous cell carcinoma (OPSCC), according to findings from a phase 2 trial presented at the 2024 American Society for Radiation Oncology (ASTRO) Multidisciplinary Head and Neck Cancers Symposium.
With a median follow-up of 32.1 months, the 2-year locoregional recurrence (LRR) rate was 6.8% (90% CI, 1.8%-11.5%) across the entire study cohort. Additionally, for patients receiving 70 Gy (n = 2), the 2-year LRR rate was 4.6% (90% CI, 0.0%-9.8%) and 9.4% (90% CI, 0.5%-17.6%) in those who received 54 Gy (n = 3).
The 2-year progression-free survival (PFS) rate in the overall population was 87% (90% CI, 81%-94%). Radiation at 70 Gy yielded a 2-year PFS rate of 89% (90% CI, 82%-97%); treatment failed 4 patients, and there was 1 death that was determined to be likely associated with treatment. Among patients who received 54 Gy of radiation, the 2-year PFS rate was 84% (90% CI, 74%-96%); treatment failed 4 patients in this group.
The median loss of weight from baseline to 3 months following radiotherapy was 23 lbs (IQR, 15-35) in the standard radiotherapy cohort compared with 11 lbs (IQR, 7-17) in the de-escalated radiation cohort (P <.001). Between radiotherapy and 1 month following treatment, feeding tube use was highlighted in 16% and 11% of patients in each respective cohort (P = .5); no patients required a feeding tube at 3 months following radiation. There were no significant changes in penetration-aspiration scale (PAS) scores in the standard and de-escalation cohorts from baseline to 3 months (P = .094) or 12 months (P = .2).
At 1 month, the difference in estimated mean University of Washington Quality of Life (UWQOL) scores in the de-escalated vs standard radiotherapy arm was –3.03, and the standardized effect size (ES) was –0.61 (P = .01). The estimated mean difference in pain subscale scores between arms was –5.98, and the standardized ES was –0.90 (P <.001).
The estimated mean difference in total Functional Assessment of Cancer Therapy-Head and Neck (FACT-HN) scores at 1 month in the de-escalated vs standard radiation arm was 9.09 with a standardized ES of 0.51 (P = .03). The estimated mean difference for the cancer subscale scores was 4.90, and the standardized ES was 0.78.
“We plan to continue to investigate the role of multimodal approaches for de-escalation of therapy for this patient population,” Samuel Regan, MD, a PGY-3 resident at The University of Michigan Radiation Oncology Residency Program, said in a presentation on these findings.
According to Regan, the study was inspired by a lack of prospectively validated predictive biomarkers for responses to CRT in patients with HPV-positive OPSCC. FDG-PET was hypothesized to be an effective imaging biomarker in this population due to findings from observational studies indicating that FDG-PET metrics during treatment correlated with oncologic end points.
The phase 2 study included patients with stage I or II p16-positive OPSCC and FDG-PET avid disease; those who received prior surgery or radiotherapy for head and neck cancer or had matted lymph nodes or cT0 disease were not able to enroll. Following a pre-treatment PET scan, patients began radiation at 70 Gy to gross disease and 56 Gy to elective lymph nodal regions concurrently with weekly carboplatin/paclitaxel. Patients then underwent a mid-treatment PET scan; those with a less than 50% decrease in metabolic tumor volume (MTV)2.5 were assigned to receive subsequent standard CRT, and those with a 50% or higher decrease in MTV2.5 were assigned to receive de-escalated CRT.
Patients in the standard CRT arm (n = 48) received 70 Gy to gross disease and 56 Gy to elective nodal regions in 35 fractions. Additionally, those in the de-escalated treatment arm (n = 36) received 54 Gy to gross disease plus 43.2 Gy to elective nodal regions in 27 fractions.
The study’s primary end point was non-inferiority of 2-year LRR rates of the entire cohort compared with those observed in a historical control group. Secondary end points highlighted in the presentation included patterns of failure and survival as well as patient-reported outcomes.
The median age was 60 years (IQR, 54-69) in the standard radiation arm and 60 years (IQR, 52-67) in the de-escalated radiation arm (P = .7). Most patients in each respective arm were male (88% vs 94%; P = .5), had stage I disease (71% vs 81%; P = .3), stage T1 disease (46% vs 47%; P = .2), and stage N1 disease (81% vs 86%; P = .7). Most patients in the standard radiation group had tumors on the tonsil (52%), and most in the de-escalated radiation arm had tumors on the base of the tongue (53%).
Reference
Regan SN, Rosen BS, Suresh K, et al. FDG-PET-based selective de-escalation of radiotherapy for HPV-related oropharynx cancer: results from a phase II trial. Presented at the 2024 American Society for Radiation Oncology Multidisciplinary Head and Neck Cancers Symposium; February 29-March 2, 2024; Phoenix, Arizona. Abstract 16.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.