- ONCOLOGY Vol 20 No 5
- Volume 20
- Issue 5
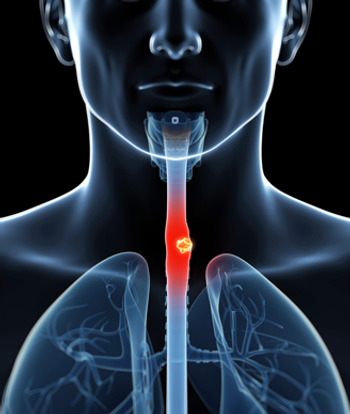
Commentary (Kleinberg et al): Primary Combined-Modality Therapy for Esophageal Cancer
Based on positive results from the Radiation Therapy Oncology Group (RTOG) 85-01 trial, the conventional nonsurgical treatment of esophageal carcinoma is combined-modality therapy. Dose intensification of the RTOG 85-01 regimen, examined in the Intergroup (INT)-0123/RTOG 94-05 trial, did not improve local control or survival. Areas of clinical investigation include the development of combined-modality therapy regimens with newer systemic agents, the use of 18F-fluorodeoxyglucose positron-emission tomography to assist in the development of innovative radiation treatment planning techniques, and the identification of prognostic molecular markers. The addition of surgery following primary combined-modality therapy apparently does not improve survival, but this finding is controversial.
Dr. Bruce Minsky presents an excellent review of data supporting nonoperative management of esophageal cancer. He describes the data in favor of primary chemoradiotherapy without surgery and concludes that combined use of chemotherapy and radiation is the standard of care for patients found to have squamous cell cancers or adenocarcinoma. While he acknowledges the conflicting data regarding treatment of each histologic type, he argues that, for now, chemoradiotherapy is appropriate for patients diagnosed with disease of either histology.
Although we agree that the evidence of benefit for adding surgery to chemoradiotherapy is controversial, the curative potential of chemoradiotherapy alone in adenocarcinoma is not yet convincingly validated. As such, nonoperative management may not be appropriate for adenocarcinoma patients who are candidates for surgical resection. Indeed, there are no models for treating adenocarcinoma of the gastrointestinal (GI) tract that show chemoradiation to be curative without surgery. For patients with operable esophageal adenocarcinoma, combined-modality therapy should include surgery. The primary question, then, becomes whether giving concomitant chemoradiation prior to surgery improves outcome.
Histologic Differences
Because esophageal squamous cell cancers and adenocarcinomas are distinct clinical entities, they must be managed differently. Each is characterized by anatomic location (upper/midesophagus vs distal esophagus/gastroesophageal junction), pattern of first failure (local vs distant), epidemiologic risk factors (tobacco and alcohol abuse vs gastroesophageal reflux disease, obesity, and diet), and patient demographics that include age, race, and comorbid conditions. In addition, a shared general approach to treatment exists for each histology that applies no matter what the location of the lesion.
When referring to squamous cell cancers, those affecting the head and neck (eg, the larynx, oropharynx, and nasopharynx) and the anus represent paradigms for which definitive chemoradiotherapy alone results in cure and organ preservation. The first trials examining nonoperative management of esophageal squamous cell cancers began in the early 1980s. This approach was based on trials using chemoradiation against squamous cell carcinoma of the anal canal that elicited exciting results.[1-3]
In contrast, surgery is the mainstay of curative treatment for adenocarcinoma arising in all anatomic sites within the GI tract. Treatment approaches for operable stages of these GI cancers focus on determining the usefulness of neoadjuvant and adjuvant therapies. Given these fundamental differences between adenocarcinoma and squamous cell cancer, perhaps esophageal adenocarcinomas and squamous cell cancers should be considered separately when discussing surgical and nonsurgical approaches.
Strides in Treatment
Over the past decade, adenocarcinoma has come to constitute the majority of esophageal cancers treated in Western industrialized countries. For locally advanced, operable disease, comprehensive staging with computed tomography (CT), endoscopic ultrasound, and positron-emission tomography most often reveals a T2 or T3 primary with N1 regional nodes and, not infrequently, M1a-designated celiac nodal involvement. In addition to this shift toward a surgically treated histology, additional changes in the recent past support the operative treatment of adenocarcinoma.
One change noted over the years is the ongoing reduction in surgical mortality. The prior high operative mortality rate of 10% to 20% motivated the development of nonsurgical treatment of esophageal cancer in the early 1980s. Over the past decade, however, mortality rates dropped below 5% at centers with experienced surgical teams.[4-6] The reason for this success is likely multifactorial, including better patient selection, improved perioperative management, and, perhaps most intriguingly, a better operative outcome in patients with adenocarcinoma compared to those with squamous cell cancer.[7-8]
Both surgical and medical principles contribute to this difference. There is a higher postoperative complication rate among patients with squamous cell cancer, perhaps because of the frequent presence of cardiopulmonary disease and the use of thoracotomy for removal of tumors in the midesophagus. In addition, patients with adenocarcinoma are more likely to undergo a microscopically complete (R0) resection.[5] This, along with pathologic stage, is the most important predictor of long-term outcome for patients treated with surgery.[7,9] Five-year survival rates range from 60% for patients with stage I disease to less than 10% for patients with stage IVA disease.[4,9] As such, adenocarcinoma is more amenable to R0 resection and, therefore, tends to have a better surgical outcome than squamous cell cancer.
When Combination Therapy Is Warranted
When surgery for locally advanced esophageal adenocarcinoma is deemed necessary, the benefit of adding neoadjuvant chemotherapy or chemoradiotherapy to surgery must be discussed. The Intergroup 0113 trial compared surgery alone with three cycles of neoadjuvant CF (cisplatin/fluorouracil) followed by surgery in 440 patients, 54% of whom had adenocarcinoma.[10] No difference in overall survival was observed when patients were stratified by treatment or histology. In both treatment groups, 60% of patients undergoing surgery had an R0 resection, and their median survival exceeded 2 years. The median survival of all randomized patients was 16 months in the surgical treatment group and 15 months in the chemotherapy/surgery group. Neoadjuvant chemotherapy not only failed to increase the R0 resection rate, but it also was associated with fewer patients undergoing surgery (80% vs 92%). This lower surgery rate combined with the lack of increase in the R0 resection rate conferred by chemotherapy may explain the absence of benefit for patients given neoadjuvant chemotherapy. As a result of this study, neoadjuvant chemotherapy added to surgery remains investigational in the United States for both adenocarcinoma and squamous cell cancer.
Neoadjuvant concomitant chemoradiotherapy, given before esophagectomy has also been tested in both histologies, but current trials from the West include mainly adenocarcinoma patients. Downstaging occurs in approximately two-thirds of patients receiving CF plus radiation, and several trials have confirmed that 25% to 30% of resected specimens have no residual tumor-defined as a pathologic complete response (pCR).[11-14] Achievement of a pCR appears to confer a survival advantage, resulting in a 60% to 70% disease-free survival rate at 5 years. Furthermore, studies that included endoscopic ultrasound and CT for rigorous pretreatment tumor-node-metastasis (TNM) staging showed that prognosis corresponds to final pathologic stage rather than initial clinical stage.[12,14-16] A further 20% to 25% of patients who are downstaged but have microscopic residual disease are 5-year survivors, confirming the importance of surgery to achieve cure.[12]
Randomized trials that address the contribution of chemoradiation added to surgery report inconsistent findings relative to survival, and thus, chemoradiotherapy followed by surgery remains controversial. Only two trials have focused on adenocarcinoma. The Walsh study from Dublin included only adenocarcinoma,[17] whereas the Urba study from the University of Michigan enrolled predominately patients with adenocarcinoma (75 adenocarcinoma, 25 squamous cell cancer).[18] Both trials showed a difference in survival at 3 years favoring chemoradiotherapy followed by surgery, but the difference was statistically significant only in the Walsh study. This research, however, has been criticized for a low survival rate (6%) in the control arm.
The Urba study showed a significant reduction in locoregional failure with chemoradiotherapy followed by surgery (19% vs 42%, P =.02) and a significant association between survival and pathologic response, with those achieving pCR living longer than those with residual tumor (3-year survival: 64% vs 19%, P = .01). A multivariate analysis showed squamous cell histology to be an independent prognostic factor for shortened survival. There was a 31% lower risk of death for patients randomized to the multimodality arm, representing only a statistical trend for benefit due to the small sample size. The Urba study results did not reach significance, but subsequent randomized studies may be difficult to undertake. As an example, an attempt to mount an adequately powered Intergroup randomized trial to answer this question in the United States was unsuccessful due to lack of patient enrollment.
In the absence of a definitive US trial, two meta-analyses provide perspective. One included nine trials and 1,116 patients[19]; the other included six trials and 746 patients.[20]. Both analyses found a statistically significant 3-year survival advantage with chemoradiotherapy followed by surgery compared with surgery alone. Other findings were a significantly higher R0 resection rate and a significant reduction in locoregional failure associated with neoadjuvant chemoradiation. The proportion of patients with adenocarcinoma, however, was too small for separate analysis by histology.
Conclusions
The question of benefit from neoadjuvant chemoradiation added to surgery will not be answered by a formal randomized trial in the United States. However, findings taken in the aggregate from phase II and III trials to date have included the ability to downstage patients and move them into a better prognostic stage category, higher R0 resection rates, and improved locoregional control. These facts argue that this approach offers operable adenocarcinoma patients the best chance for long-term survival. Until available data demonstrate otherwise, a nonsurgical approach for localized, resectable esophageal adenocarcinoma should be limited to medically unfit patients. In the future, the identification of molecular prognostic markers should sharpen our ability to predict outcome, improve patient selection, and expand therapeutic strategies.
-Lawrence Kleinberg, MD
-Michael Gibson, MD
-Stephen Yang, MD
-Arlene A. Forastiere, MD
Disclosures:
Dr. Minsky is a consultant and speaker for Sanofi-Aventis and Roche; and is a consultant and speaker for, and receives research funding from Genentech and Bristol-Myers Squibb.
References:
1. Nigro ND, Vaitkevicius VK, Buroker T, et al: Combined therapy for cancer of the anal canal. Dis Colon Rectum 24:73-75; 1981.
2. Franklin R, Steiger Z, Vaishampayan G, et al: Combined modality therapy for esophageal squamous cell carcinoma. Cancer 51:1062-1071, 1983.
3. Leichman L, Herskovic A, Leichman CG, et al: Nonoperative therapy for squamous-cell cancer of the esophagus. J Clin Oncol 5:365-70, 1987.
4. Orringer MB, Marshall B, Iannettoni MD: Transhiatal esophagectomy for treatment of benign and malignant esophageal disease. World J Surg 25:196-203, 2001.
5. Doty JR, Salazar JD, Forastiere AA, et al: Postesophagectomy morbidity, mortality, and length of hospital stay after preoperative chemoradiation therapy. Ann Thorac Surg 74:227-231, 2002.
6. Stein HJ, Siewert JR: Improved prognosis of resected esophageal cancer. World J Surg 28:520-525, 2004.
7. Siewert JR, Stein HJ, Feith M, et al: Histologic tumor type is an independent prognostic parameter in esophageal cancer: Lessons from more than 1,000 consecutive resections at a single center in the Western world. Ann Surg 234:360-367, 2001.
8. Orringer MB, Marshall B, Iannettoni MD: Transhiatal esophagectomy: Clinical experience and refinements. Ann Surg 1230:392-400, 1999.
9. Law S, Kwong DL, Kwok KF, et al: Improvement in treatment results and long-term survival of patients with esophageal cancer: Impact of chemoradiation and change in treatment strategy. Ann Surg 238:339-347, 2003.
10. Kelsen DP, Ginsberg R, Pajak TF, et al: Chemotherapy followed by surgery compared with surgery alone for localized esophageal cancer. N Engl J Med 339:1979-1984, 1998.
11. Forastiere AA, Orringer MB, Perez-Tamayo C, et al: Preoperative chemoradiation followed by transhiatal esophagectomy for carcinoma of the esophagus: Final report. J Clin Oncol 11:1118-1123, 1993.
12. Kleinberg L, Knisely JP, Heitmiller R, et al: Mature survival results with preoperative cisplatin, protracted infusion 5-fluorouracil, and 44-Gy radiotherapy for esophageal cancer. Int J Radiat Oncol Biol Phys 56:328-334, 2003.
13. Swisher SG, Ajani JA, Komaki R, et al: Long-term outcome of phase II trial evaluating chemotherapy, chemoradiotherapy, and surgery for locoregionally advanced esophageal cancer. Int J Radiat Oncol Biol Phys 57:120-127, 2003.
14. Berger adenocarcinoma, Farma J, Scott WJ, et al: Complete response to neoadjuvant chemoradiotherapy in esophageal carcinoma is associated with significantly improved survival. J Clin Oncol 23:4330-4337, 2005.
15. Chirieac LR, Swisher SG, Ajani JA, et al: Posttherapy pathologic stage predicts survival in patients with esophageal carcinoma receiving preoperative chemoradiation. Cancer 103:1347-1355, 2005.
16. Heath EI, Burtness BA, Heitmiller RF, et al: Phase II evaluation of preoperative chemoradiation and postoperative adjuvant chemotherapy for squamous cell and adenocarcinoma of the esophagus. J Clin Oncol 18:868-876, 2000.
17. Walsh TN, Noonan N, Hollywood D, et al: A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med 335:462-467, 1996.
18. Urba SG, Orringer MB, Turrisi A, et al: Randomized trial of preoperative chemoradiation versus surgery alone in patients with locoregional esophageal carcinoma. J Clin Oncol 19:305-313, 2001.
19. Urschel JD, Vasan H: A meta-analysis of randomized controlled trials that compared neoadjuvant chemoradiation and surgery to surgery alone for resectable esophageal cancer. Am J Surg 185:538-543, 2003.
20. Fiorica F, Di Bona D, Schepis F, et al: Preoperative chemoradiotherapy for oesophageal cancer: A systematic review and meta-analysis. Gut 53:925-930, 2004.
Articles in this issue
almost 20 years ago
Whatever It Takesalmost 20 years ago
Docetaxel Approved for Advanced Stomach Canceralmost 20 years ago
Primary Combined-Modality Therapy for Esophageal Canceralmost 20 years ago
Adjuvant Therapy for Colorectal Cancer: Yesterday, Today, and Tomorrowalmost 20 years ago
Rituximab Effective in Treating Chronic Graft-vs-Host Diseasealmost 20 years ago
Fertility-Preserving Options for Cervical Canceralmost 20 years ago
Commentary (Putnam): Primary Combined-Modality Therapy for Esophageal Canceralmost 20 years ago
Commentary (Kuban): Permanent Prostate BrachytherapyNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.