Oncology NEWS International
- Oncology NEWS International Vol 13 No 5
- Volume 13
- Issue 5
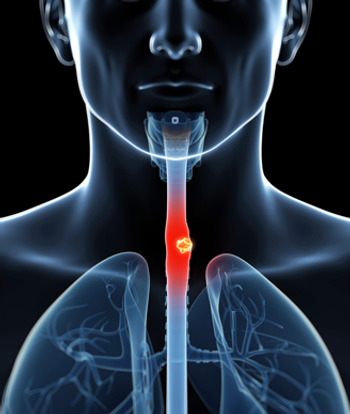
Esophageal Ca: No Benefit From Preop Chemo-RT
NEW YORK-A retrospective review of 10 years of data on patients who underwent surgical resection for esophageal cancer has shown no survival advantage for patients who had a complete pathologic response to neoadjuvant chemoradiation followed by surgery vs those who had surgery alone. In light of this finding, the researchers suggest that other therapeutic avenues be explored for patients with locally advanced esophageal cancer.
NEW YORKA retrospective review of 10 years of data on patients who underwent surgical resection for esophageal cancer has shown no survival advantage for patients who had a complete pathologic response to neoadjuvant chemoradiation followed by surgery vs those who had surgery alone. In light of this finding, the researchers suggest that other therapeutic avenues be explored for patients with locally advanced esophageal cancer.
Carl R. Schmidt, MD, a research fellow in surgical oncology, Department of Surgery, Vanderbilt University Medical Center (VUMC), reported the results on behalf of colleagues from VUMC, Vanderbilt-Ingram Cancer Center, and Nashville Veteran’s Administration Hospital, at the Society of Surgical Oncology 57th Annual Cancer Symposium
(abstract 17).
The investigators undertook this study, Dr. Schmidt said, because trials and meta-analyses in the medical literature show conflicting data on both survival benefit and perioperative morbidity and mortality from preoperative neoad-juvant chemoradiation vs surgical resection alone in patients with esophageal cancer.
Included in the study were 147 patients with stages I to III esophageal cancer who underwent esophagectomy with curative intent between 1992 and 2002. Of these 147 patients, 119 had both neo-adjuvant chemoradiation therapy and surgery, and 28 were treated with surgery alone. Patients had either adenocarcinoma (n = 106) or squamous cell carcinoma (n = 41). Excluded were patients who had metastatic disease (stage IV), palliative surgery for esophageal cancer, or resection for high-grade dysplasia.
Four different regimens were used for neoadjuvant chemoradiation during the study period, as some of the patients were enrolled in phase I and II trials, Dr. Schmidt said. Clinical stage was determined by abdominal and chest CT scans; endoscopic ultrasound was performed in 64 patients (44%). A "complete response" (CR) was defined as no evidence of tumor in the resected specimen at the time of surgery, and "no CR" was defined as any gross or microscopic residual tumor in the pathologic specimen.
The median follow-up time for the patients was 21 months overall and 26 months for survivors. The investigators noted a CR in 32% of patients who underwent neoadjuvant chemoradiation, a result comparable to other reported studies. In the Tennessee study, however, no significant differences were seen in overall disease-specific survival (median, 35.9 months with CR vs 29.6 months with no CR, P = .17) or disease-free survival (median, 37.7 months with CR vs 26.5 months with no CR, P = .29) between patients who had a CR to preoperative chemoradiation vs those who did not: Kaplan-Meier survival plots for the two patient groups were similar, with actuarial curves for overall survival estimated at about 30%.
Independent prognostic factors for worse survival in patients who had neo-adjuvant therapy and surgical resection included late clinical stage, as expected, and, unexpectedly, a transthoracic vs transhiatal approach (transthoracic surgery is usually associated with improved survival). Dr. Schmidt stressed that only 20% of patients in the neoadjuvant group received transthoracic surgery, and he said a trend toward increased surgical morbidity and mortality in the transthoracic patients might explain the finding.
A subgroup analysis of patients with later-stage vs earlier-stage disease showed no difference in overall disease-specific or disease-free survival for earlier-stage patients with CR vs no CR to neoadjuvant therapy. In the later-stage patients, however, there appeared to be "a trend toward improved survival with a complete response . . . to neoadjuvant therapy, although this did not reach statistical significance," he said.
In assessing the entire cohort, using a Cox proportional hazards model to determine prognostic factors for survival, again, late clinical stage at presentation and transthoracic approach predicted a worse overall survival in all patients, while use of neoadjuvant therapy was not a significant predictor for survival.
Morbidity and mortality in the two treatment groups were comparable: "Our overall perioperative mortality was six patients, or 3.9%," Dr. Schmidt said. "We saw no differences in mortality, overall complications, or major complications between those who had surgical resection alone vs those who underwent preoperative chemoradiation with surgical resection. An exception to that was a surprising higher rate of leak in our patients who underwent surgical resection alone vs the neoadjuvant group, but our overall leak rate was fairly low at 7%."
Dr. Schmidt concluded: "We believe continued assessment of the value of neoadjuvant therapy in esophageal cancer is necessary, including prospective randomized trials, molecularly targeted therapies, and other avenues of therapy."
Limitations to the study, Dr. Schmidt noted, include the fact that patients received a variety of chemoradiation regimens but separate assessments were not made in evaluating responses. "If there was one regimen that was more effective than the others, its effect would have been diluted by our decision to include all patients," he said.
Other possible limitations included the fact that the investigators could not know whether preoperative T stage was well-matched between the groups that did or did not receive neoadjuvant chemoradiation, because more than half of the patients did not have an endoscopic ultrasound. The procedure was not widely used at VUMC in the earlier years for which data were collected, so some patients may have been understaged.
"Given that we saw a trend toward improved survival in late-stage patients," Dr. Schmidt said, "perhaps if the staging of our patients had been more late-stage rather than early-stage patients, we might have seen an overall survival benefit."
Another limiting factor may have been lack of standardization over the 10-year period in the pathologic assessment of esophageal cancer specimens and the criteria for designating "complete response." At VUMC, Dr. Schmidt noted, beginning in 1996, a rigorous protocol for assessment of response was instituted that included much more careful sectioning of esophageal tumors and very close inspection of the gastroesophageal junction. It is possible, he said, that prior to 1996, some patients may have been inappropriately assessed as having had a complete response.
Finally, chemoradiation itself may alter patterns of recurrence in esophageal cancer, Dr. Schmidt said. Findings previously reported by the VUMC group showed "some strange patterns of recurrence that specifically included some of our patients who had a complete response, including first recurrences in bone, brain, and soft-tissue locations that seemed unusual first-recurrence sites for this disease; 78% of our recurrences were distal, not locoregional," he said. "We think perhaps that chemoradiation therapy changes the biology of the disease and patterns of recurrence. This may explain some of the survival results seen in our studies and others. This is something that we should look at further."
Articles in this issue
almost 22 years ago
Ductal Lavage to Detect Breast Ca Questionedalmost 22 years ago
New Study Shows Higher CVD Mortality in Breast Cancer Patients Receiving RTalmost 22 years ago
Exemestane Bests Tam in Metastatic Breast CancerNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.