Experimental FLT3 Inhibitor May Benefit Patients with Refractory AML
An FLT3 inhibitor, gilteritinib, has been found to result in more frequent and sustained responses in patients with relapsed, refractory acute myeloid leukemia.
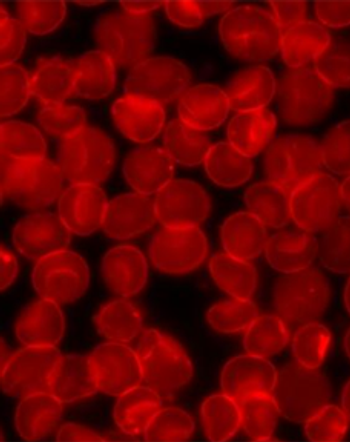
Clinicians may soon have a new tool to aid patients with refractory acute myeloid leukemia (AML). Researchers at the Perelman School of Medicine at the University of Pennsylvania and Penn’s Abramson Cancer Center
The authors noted that the FLT3 mutation is one of the most common mutations in AML, and it is associated with relapse and short survival, so this study shows promise for a particularly vulnerable patient population. “FLT3 mutations are both prognostically and therapeutically important in AML. Here, we have shown that gilteritinib, a selective, potent FLT3 inhibitor has substantial clinical efficacy with limited toxicity in relapsed FLT3 mutated patients, including patients with mutations that confer resistance to other drugs in this class,” said lead study author Alexander Perl, MD, assistant professor of Hematology Oncology at Penn’s Abramson Cancer Center in Philadelphia, Pennsylvania.
In this phase I study, researchers administered gilteritinib at increasing doses in patients who had AML that relapsed or was no longer responding to chemotherapy. Among the 252 patients in this study, 67 were on a 120-mg dose and 100 were on a 200-mg dose.
Among the 252 patients, 191 had an FLT3 mutation; overall, 49% of patients with the mutation showed a response. Just 12% of patients who didn’t have the mutation responded to the drug. The researchers found that 100 (40%) of 249 patients in the full analysis set achieved a response, with 19 patients (8%) achieving complete remission. They also discovered that 10 patients (4%) achieved a complete remission with incomplete platelet recovery, 46 patients (18%) had complete remission with incomplete hematologic recovery, and 25 patients (10%) experienced partial remission.
“Gilteritinib-treated patients were primarily managed in the outpatient setting taking a once-a-day pill. A phase III study to determine whether single-agent gilteritinib improves survival compared to standard chemotherapy regimens is ongoing. Studies of gilteritinib as part of frontline therapy of FLT3-mutated AML have also been initiated,” Dr. Perl told OncoTherapy Network.
The drug was generally well tolerated. The three most common side effects attributed to the drug were diarrhea in 41 patients (16%), fatigue in 37 patients (15%), and abnormal liver enzyme tests in 33 patients (13%). “With the exception of patients receiving the highest doses of gilteritinib, side effects only rarely prompted dose reduction. Current phase III trials are using 120-mg dosing, which is very well tolerated and seldom needs dose reduction,” said Dr. Perl.
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.