
FDA OKs Brentuximab Vedotin Combo in R/R Large B-Cell Lymphoma
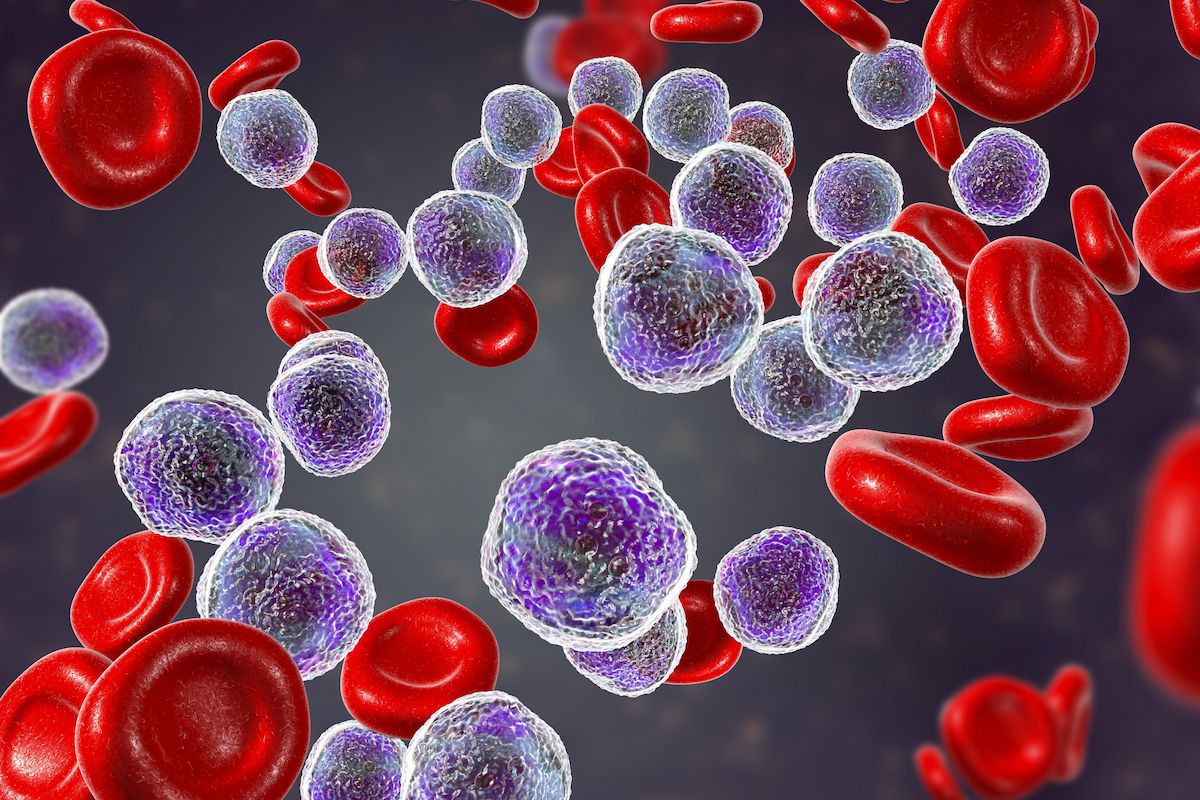
Data from the ECHELON-3 trial support the approval of the brentuximab vedotin combo in relapsed/refractory B-cell lymphoma.
The FDA has approved brentuximab vedotin (Adcetris) plus lenalidomide (Revlimid) and rituximab (Rituxan) for patients with relapsed/refractory large B-cell lymphoma (LBCL), according to a news release from the agency.1
Specifically, the indication extends to those with diffuse large B-cell lymphoma (DLBCL) not otherwise specified, DLBCL resulting from indolent lymphoma, or high-grade B-cell lymphoma (HGBL) following at least 2 prior lines of treatment who are ineligible to receive CAR T-cell therapy or autologous hematopoietic stem cell transplantation (auto-HSCT).
Supporting data for the approval came from the double-blind
Findings from the ECHELON-3 trial were previously published in the Journal of Clinical Oncology.2 Additional data showed a median duration of response (DOR) of 8.3 months (95% CI, 4.2-15.3) in the brentuximab vedotin group and 3.0 months (95% CI, 2.8-5.4) in the placebo group.
Regarding safety, treatment-emergent AEs (TEAEs) of any grade occurred in 97% of patients who received brentuximab vedotin vs 97% of patients in the placebo arm; TEAEs of grade 3 or higher occurred in 88% and 77%, respectively. The most common TEAEs of grade 3 or higher in each arm included neutropenia (43% vs 28%), thrombocytopenia (25% vs 19%), anemia (22% vs 21%), and pneumonia (11% vs 5%).
The trial’s primary end point was OS. Key secondary end points included PFS, ORR, complete response rate, DOR per Lugano classification, and AEs.
The agency approved brentuximab vedotin at a recommended dose of 1.2 mg/kg up to 120 mg in combination with lenalidomide and rituximab every 3 weeks until progressive disease or unacceptable toxicity.
References
- FDA approves brentuximab vedotin with lenalidomide and rituximab for relapsed or refractory large B-cell lymphoma. News release. FDA. February 11, 2025. Accessed February 12, 2025. https://tinyurl.com/4mhcnndc
- Bartlett NL, Hahn U, Kim W-S, et al. Brentuximab vedotin combination for relapsed diffuse large B-cell lymphoma. J Clin Oncol. Published online January 7, 2025. doi:10.1200/JCO-24-02242
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.



































