- ONCOLOGY Vol 24 No 3
- Volume 24
- Issue 3
Lessons Learned From the Use of ESAs
Dr. Bennett and colleagues have provided a thorough and balanced history of the rise and fall of erythropoietin-stimulating agents (ESAs) in cancer-associated anemia. Their review encourages us to think about the lessons learned from this history-lessons about medical progress, the importance of clinical research in guiding clinical practice, and the role of the US Food and Drug Administration (FDA) in protecting patients
Dr. Bennett and colleagues have provided a thorough and balanced history of the rise and fall of erythropoietin-stimulating agents (ESAs) in cancer-associated anemia.
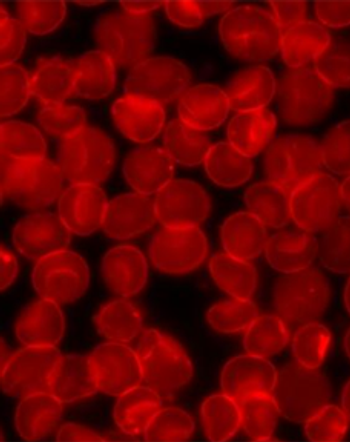
In 1993, the ESAs were first approved for management of treatment-associated anemia in patients with nonmyeloid malignancies. Pooled data from six randomized trials of ESAs in patients with solid tumors treated with chemotherapy showed that administration of ESAs decreased the need for red cell transfusion (22%) compared with the placebo arm (43%). In 2002, based on similar results from use of the longer-acting ESAs administered less frequently (51% vs 21% transfusions), darbepoetin alfa (Aranesp) was approved.[1] Physicians and patients were anxious to avoid red blood cell transfusions in the wake of the AIDS epidemic and the concern about hepatitis C transmission, for which there was no screening test.
In a report published in the New England Journal of Medicine in 1996,[2] the risk of transfusion-transmitted viral infection was estimated on a population of over one-half million screened donors who had contributed more than 1 unit of blood between 1991 and 1993. Risk of infection was calculated based on the incidence of seroconversion over time among these individuals. The risk of HIV transmission was estimated to be 1 in 493,000, risk of hepatitis C transmission was 1 in 103,000, and risk of hepatitis B transmission was 1 in 63,000.[2] By 2003, the safety of our blood banks had so improved that the risk of HIV transmission had decreased to < 1 in 1 million, risk for hepatitis C had dropped to < 1 in 1 million, and risk for hepatitis B was reduced to < 1 in 400,000.[3] By improving the safety of blood products, the impetus to avoid transfusion decreased.
Lesson 1: Competing Improvements in Clinical Care May Change the Significance of an Intervention
Cancer-related fatigue is reported by more than 60% of patients receiving chemotherapy.[4-6] This fatigue is debilitating and significantly compromises the quality of life of patients. While every patient is assessed clinically as an individual, transfusion medicine specialists generally recommend that patients with chronic anemia maintain hemoglobin levels in excess of 7 to 8 g/dL. Yet the level of self-reported fatigue has been shown to be inversely related to the hemoglobin level even at levels in excess of 8 g/dL.[7] Using the Surveillance Epidemiology and End Results (SEER)-Medicare database, Hershman identified more than 56,000 patients who were treated with chemotherapy for cancers of the colon, non–small-cell lung cancer (NSCLC), breast, and diffuse large cell lymphoma from 1991 to 2002.[8] While use of ESAs in this population increased after drug approval, the rate of transfusions was unchanged. In clinical practice the use of ESAs was expanded to maintain hemoglobin levels in excess of what would normally dictate a red cell transfusion, on the presumption that cancer-related fatigue would be minimized.
The clinical data that were used to support use of ESAs in treatment of cancer-related fatigue were largely derived from open-label randomized trials in patients with a variety of malignancies, at different stages of disease, and receiving different cytotoxic therapies. As Dr. Bennett and his coauthors point out, the “FDA statisticians concluded that [quality of life] claims by manufacturers for cancer patients were not statistically valid.”
Lesson 2: There Is No Substitute for a Well-Designed, Randomized, Double-Blind, Placebo-Controlled Trial
It is of note that a Cochrane review entitled “Drug Therapy for the Management of Cancer-Related Fatigue” concluded that the ESAs “are effective in the management of cancer-related fatigue in patients who are anemic as a result of chemotherapy.” However, the authors caution that “These drugs are not without side effects and they should be used under expert supervision and their effect closely monitored.”[9]
The FDA was concerned about the impact of the ESAs on cancer outcomes and reviewed the safety data at an Oncologic Drugs Advisory Committee (ODAC) meeting in May 2004. At that time, the FDA determined that two studies-a small-cell lung cancer trial (N93-004) and the Breast Cancer Erythropoietin Survival Trial (BEST)-were adequately designed to evaluate ESA safety and cancer outcomes. The committee concluded that further studies were needed to determine if ESAs had an effect on cancer-specific outcomes. No change in ESA use was recommended.
The ESAs continued to be used in patients with cancer, chronic renal failure, and in individuals undergoing orthopedic surgical procedures. With additional safety data and before the next ODAC review in May 2007, the FDA issued three separate public health advisories in November 2006, January 2007, and February 2007. These advisories raised safety concerns and cautioned that the target hemoglobin level should not exceed 12 g/dL. Later in 2007, a Black Box warning identified venous thromboembolic events (VTEs) as a complication related to ESAs.
Lesson 3: All Treatment Interventions Have Potential Side Effects
By the May 2007 ODAC meeting, adequate safety and outcome data were available from six clinical trials. The ESAs were associated with a decrease in overall survival in patients with both myeloid and nonmyeloid malignancies, as well as a decrease in local regional control of head and neck cancer and NSCLC, and an increased risk of VTEs was again observed.[1] With these additional data, the committee recommended that ESAs be avoided in patients with potentially curative malignancies.
All ODAC meetings include an “Open Public Hearing” at which advocates provide testimony regarding the questions posed to the committee. The May 2007 meeting was particularly emotional as cancer advocates with metastatic disease questioned whether the use of ESAs during adjuvant therapy had “caused” their cancer recurrence. It is clear that additional studies will be needed to clarify whether the adverse effects of ESAs are unique to characteristics of cancer cells, too high a hemoglobin goal (> 12 g/dL), host effects, or other factors.
Lesson 4: The Systems in Place to Protect Our Patients Do Work
Until the aforementioned issues have been satisfactorily clarified, patients who are at risk for an adverse outcome do not receive ESAs, as reinforced by the review by Dr. Bennett et al. A clear lesson in the changing use of ESAs in cancer patients is the importance of evidence-based medicine as a guide for clinical practice, and the shift in recommended indications for ESAs shows that the systems in place to protect our patients do work.
References:
References
1. Juneja V, Keegan P, Gootenberg JE, et al: Continuing reassessment of the risks of erythropoiesis-stimulating agents in patients with cancer. Clin Cancer Res 14:3242-3247, 2008.
2. Schreiber GB, Busch MP, Kleinman SH, et al: The risk of transfusion-transmitted viral infections. N Engl J Med 334:1685-1690, 1996.
3. Dzik W: Emily Cooley Lecture 2002: Transfusion safety in the hospital. Transfusion 43:1190-1199, 2003.
4. Servaes P, Verhagen C, Bleijenberg G: Relations between fatigue, neuropsychological functioning, and physical activity after treatment for breast carcinoma. Cancer 95:2017-2026, 2002.
5. Servaes P, Verhagen C, Bleijenberg G: Fatigue in cancer patients during and after treatment: Prevalence, correlates and interventions. Eur J Cancer 38:27-43, 2002.
6. Iop A, Manfredi AM, Bonura S: Fatigue in cancer patients receiving chemotherapy: An analysis of published studies. Ann Oncol 15:712-720, 2004.
7. Cella D, Eton DT, Lai J-S, et al: Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue Scales.
J Pain Symptom Manage 24:547-561, 2002.
8. Hershman DL, Buono DL, Malin J, et al: Patterns of use and risks associated with erythropoiesis-stimulating agents among Medicare patients with cancer. J Natl Cancer Inst 101:1633-1641, 2009.
9. Minton O, Richardson A, Sharpe M, et al: A systematic review and meta-analysis of the pharmacological treatment of cancer-related fatigue. J Natl Cancer Inst 100:1155-1166, 2008.
Articles in this issue
almost 16 years ago
FDA Approves Rituximab for Chronic Lymphocytic Leukemiaalmost 16 years ago
The Many Controversies of Stage IIIA/IIIB Lung Canceralmost 16 years ago
A Young Woman With Multiple Kidney Lesionsalmost 16 years ago
FDA Cancer Drug Approval Rate Highlighted in JNCIalmost 16 years ago
Nilotinib Gets Priority Review for Newly Diagnosed Early CMLalmost 16 years ago
Lycopenealmost 16 years ago
Further Considerations in the Treatment of Locally Advanced Lung Canceralmost 16 years ago
Reassessments of ESAs for Cancer Treatment in the US and EuropeNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.