- ONCOLOGY Vol 10 No 9
- Volume 10
- Issue 9
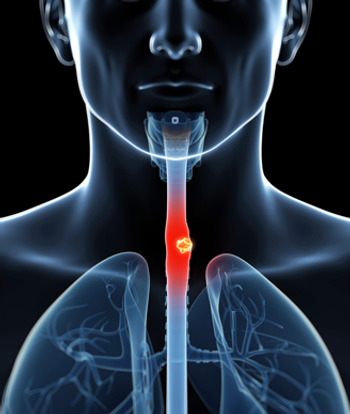
Management of Esophageal Cancer
Drs. Ilson and Kelsen present an excellent review of the current investigations and treatment recommendations for patients with esophageal cancer. In a comprehensive and concise fashion, they detail controversies in surgical and nonsurgical management, neoadjuvant therapies, and regimens for treating metastatic disease. Their review provides an opportunity to further highlight several research questions.
Drs. Ilson and Kelsen present an excellent review of the currentinvestigations and treatment recommendations for patients withesophageal cancer. In a comprehensive and concise fashion, theydetail controversies in surgical and nonsurgical management, neoadjuvanttherapies, and regimens for treating metastatic disease. Theirreview provides an opportunity to further highlight several researchquestions.
Anatomic Considerations and Natural History
When esophageal cancer is initially treated for cure with onelocal treatment modality (surgery or radiotherapy), treatmentfailure is due to both local and distant disease and both contributeto mortality. This is important to keep in mind when designingtrials to improve survival. Early distant spread is explainedby the dense network of lymphatics in the mucosa and submucosathat interconnect with lymphatic vessels in the muscular layersof the esophagus. These lymphatic channels drain primarily longitudinallyto regional and distant nodal beds. Local recurrence is also tobe expected because circumferential "margins" of resectionare nearly always positive for microscopic tumor, whereas proximaland distal margins of resection, provided in the surgical pathologyreport, are usually negative.
Thus, it does make sense that utilizing all three modalities--radiationtherapy and surgery for local control and chemotherapy for distantspread--would offer the best chance for cure in a patient presentingwith localized disease. Surgery is the most effective means fordebulking the primary tumor or eradicating residual disease inthe esophagus after preoperative therapy. It makes sense to addradiotherapy to surgery to improve local control, particularlyfor patients with T3 and T4 disease, in whom residual microscopicdisease in the tumor bed is likely. Chemotherapy certainly hasa role in enhancing the effects of radiation and as a systemictherapy for occult distant spread. The critical question is howto optimally sequence these three therapies to cure or significantlyincrease survival time in the highest percentage of patients whopresent with potentially curable localized disease.
Surgery Combined With Radiotherapy
Controlled trials of surgery combined with preoperative or postoperativeradiotherapy do not demonstrate an improvement in survival andare conflicting with regard to the effects of this combinationon locoregional control. One trial of preoperative radiotherapyshowed a decrease in locoregional failure (46% vs 67%), but othersshowed no effect.[1-4] Postoperative radiotherapy has a high rateof toxicity to normal tissues because of the potentially largevolumes irradiated.
Only two controlled trials of surgery combined with postoperativeradiotherapy are available.[5,6] One trial showed a reductionin locoregional failure in a subset analysis of pathologicallystaged N0 patients, and the other, which involved patients whohad all gross tumor removed and negative resection margins, showedno effect.
Surgery Combined With Chemotherapy
Because distant metastasis is a major cause of death and earlyfailure in patients with esophageal cancer, the addition of preoperative(neoadjuvant) systemic therapy to surgery makes intuitive sense.The limitation of this two-modality approach is that only 50%of tumors are sensitive to current cisplatin (Platinol)-basedchemotherapy regimens and pathologic complete response is infrequent.This situation is in contrast to squamous cell cancer of the headand neck (after which these esophageal trials were modeled), inwhich 80% to 90% of patients respond and 30% to 50% may achievea pathologic complete response. This is a major weakness in thistreatment strategy and diminishes the possibility that adjunctivechemotherapy will have sufficient impact on locoregional failureand distant metastasis rates to significantly improve survivalover surgery alone.
The GI Intergroup Trial, which enrolled over 400 patients andis now undergoing analysis, will provide a definitive answer tothe question of whether the combination of preoperative chemotherapyand surgery affords a survival benefit. In addition, this trialwas open to patients with adenocarcinoma of the esophagus, aswell as squamous cell carcinoma, so that for the first time comparisonscan be made between the two histologic types with statisticalconfidence. This information and that gleaned from various subsetanalyses should yield important insights for future trial design.Until the data analysis of this critically important trial ismature, surgery remains the standard of care for patients withlocalized disease.
Currently, the role of postoperative adjuvant chemotherapy orchemoradiation is undefined. There are no data to suggest thatadministering postoperative adjuvant chemotherapy prolongs eitherthe disease-free interval or survival, particularly in patientswho have undergone a curative resection and have negative nodes.Patients who have positive margins of resection, however, shouldbe considered for postoperative radiation.
Concurrent Chemotherapy and Radiotherapy Without Surgery
Survival benefit has clearly been established for concurrent chemotherapyand radiotherapy, compared to radiotherapy alone, in patientswith squamous cell cancer, but this has not been adequately addressedin patients with adenocarcinoma. This conclusion is supportedby the intergroup trial results published by Herskovic, Al-Sarraf,and colleagues.[7,8] Despite improved survival (median survival,14 months; 3-year survival rate, 30%) in patients treated withchemoradiation, the rate of persistent or recurrent disease inthe esophagus at 1 year was unacceptably high.
Results from nonsurgical trials indicate that local failure occursin at least 45% to 50% of patients.[7,9,10] This is of particularconcern when treating patients with localized, potentially curabledisease. For most patients, chemoradiation (cisplatin, fluorouracil[5-FU], or mitomycin [Mutamycin] with 50 to 60 Gy of radiation)alone will not irradicate bulk disease in the esophagus. Thus,oncologists should not be satisfied with this therapy as "recommendedtreatment" except for patients with disease extending outsideof the esophagus into adjacent structures (T4) or those with medicalrisks that preclude resection.
No doubt, there is a subset of patients with squamous cell cancerwho can be cured without surgery. Identifying these patients posesa challenge since we know that the results of endoscopic biopsygreatly overestimate the pathologic complete response rate whencompared to resection specimens.[11,12] Esophageal endoscopicultrasound is being studied for its accuracy in predicting completeresponse but is unlikely to be able to accurately discriminatetumor given the degree of acute tissue injury and subsequent fibrosisthat occur after chemotherapy and radiotherapy. The best way toaddress the question is with very careful staging that includesendoscopic ultrasound, radiologic imaging, and laparoscopy fordistal lesions before patients enter a controlled trial. It maythen be feasible to identify patient subgroups who are likelyto be cured without surgery.
Concurrent Chemotherapy and Radiotherapy Followed by Surgery
Drs. Ilson and Kelsen discuss several published trials of concurrentchemoradiation followed by surgery that were conducted in the1980s. Pilot trials from Wayne State University, the SouthwestOncology Group (SWOG), and the Radiation Therapy Oncology Group(RTOG), which entailed the administration of two courses of cisplatin,with or without 5-FU, combined with 30 Gy of radiation, reportedpathologic complete response rates in 25% to 30% of patients andsuggested a survival advantage for pathologic complete responders.Most patients died from distant disease without local recurrence.This finding lends support to the importance of removing the esophagus,which, in 50% to 70% of patients, harbors residual disease.
The preponderence of distant disease indicates a need for improvedsystemic therapy. The data published from the University of Michigan,[13]Johns Hopkins,[14,15] and, most recently, the University of NorthCarolina[11] support this alternative interpretation of the resultsof those early trials cited by Dr. Ilson and Dr. Kelsen in theirreview. Using protracted low-dose infusional 5-FU and continuous-infusioncisplatin with concurrent radiotherapy, comparable results fromtwo sequential pilot trials (total of 93 patients) have been publishedby Forastiere and colleagues: median survivals of 29 and 31 months,respectively; 2-year survival rates of 57% and 58%, respectively;and long-term survival in approximately 30% of patients with residualtumor in the resected esophagus and in 60% of pathologic completeresponders.[13-15] Bates, Tepper, and colleagues reported a mediansurvival of 26 months, 2-year survival rate of 53%, and survivalbeyond 3 years in 25% of patients with tumor in the resected esophagealspecimen and in 61% of pathologic complete responders.[11]
These and other recently published trials not included in Table2 of this review support the need for further evaluation of thethree-modality approach in large randomized trials.[16-19] Localcontrol was observed in 75% to 90% of patients in these trialsand appears to be optimized. The challenge is to find alternative,more effective systemic therapies to decrease distant metastases.Controlled trials that accrue large numbers of patients are neededso that clinically meaningful survival differences can be demonstratedwith statistical confidence. This has yet to be done. A comparisonof preoperative chemoradiation followed by surgery to surgeryalone and a comparison of a surgical to a nonsurgical multimodalityapproach are two randomized trials that need to be conducted.
Until these trials have been carried out, these multimodalityapproaches must be considered experimental. Patients will be affordedthe best outcome if treated at centers that have a dedicated multidisciplinaryteam and a formal esophageal cancer research program.
References:
1. Arnott SJ, Duncan W, Kerr GR, et al: Low dose preoperativeradiotherapy for carcinoma of the oesophagus: Results of a randomizedclinical trial. Radiother Oncol 24:108-113, 1992.
2. Nygaard K, Hagen S, Hansen HS, et al: Pre-operative radiotherapyprolongs survival in operable esophageal carcinoma: A randomized,multicenter study of pre-operative radiotherapy and chemotherapy.The second Scandinavian trial in esophageal cancer. World J Surg16:1104-9, 1992.
3. Mie W, Xian-Zhi G, Weibo Y, et al: Randomized clinical trialon the combination of preoperative irradiation and surgery inthe treatment of esophageal carcinoma: A report of 206 patients.Int J Radiat Oncol Biol Phys 16:325-327, 1989.
5. Gignoux M, Roussel A, Paillot B, et al: The value of preoperativeradiotherapy in esophageal cancer: Results of a study of EORTC.World J Surg 11:426-432, 1987.
6. Fok M, Sham JST, Choy D, et al: Postoperative radiotherapyfor carcinoma of the esophagus: A prospective, randomized controlledstudy. Surgery 113(2):138-147, 1996.
7. Herskovic A, Martz K, Al-Sarraf M, et al: Combined chemotherapyand radiotherapy compared with radiotherapy alone in patientswith esophageal cancer. Proc Am Soc Clin Oncol 12:580, 1993.
8. Al-Sarraf M, Martz K, Herskovic A, et al: Superiority of chemo-radiotherapy (CT-RT) vs radiotherapy (RT) in patients with esophagealcancer: Final report of an intergroup randomized and confirmedstudy. Proc Am Soc Clin Oncol 15:206, 1996.
9. Coia LR, Engstrom PF, Paul AR, et al: Long-term results ofinfusional 5-FU, mitomycin-C and radiation as primary managementof esophageal carcinoma. Int J Radiat Oncol Biol Phys 20:29-36,1991.
10. Leichman L, Herskovic A, Leichman CG, et al: Nonoperativetherapy for squamous-cell cancer of the esophagus. J Clin Oncol5:365-370, 1987.
11. Bates BA, Detterbeck FC, Bernard SA, et al: Concurrent radiationtherapy and chemotherapy followed by esophagectomy for localizedesophageal carcinoma. J Clin Oncol 14(1):156-163, 1996.
12. Leichman L. Cancer of the esophagus: The Wayne State Universityexperience. Investigational New Drugs 7:91-100, 1989.
13. Forastiere AA, Orringer MB, Perez-Tamayo C, et al: Preoperativechemoradiation followed by transhiatal esophagectomy for carcinomaof the esophagus: Final report. J Clin Oncol 11:1118-1123, 1993.
14. Forastiere AA, Heitmiller R, Lee DJ, et al: A 4 week intensivepreoperative chemoradiation program for logoregional cancer ofthe esophagus. Proc Am Soc Clin Oncol 13:195, 1994.
15. Forastiere AA, Heitmiller RF, Lee DJ, et al: Intensive chemoradiationfollowed by esophagectomy for squamous cell and adenocarcinomaof the esophagus (submitted for publication).
16. Malhaire JP, Labat JP, Lozach P, et al: Preoperative concomitantradiochemotherapy in squamous cell carcinoma of the esophagus:Results of a study of 56 patients. Int J Radiat Oncol Biol Phys34(2):429-437, 1996.
17. Stahl M, Wilke H, Fink U, et al: Combined preoperative chemotherapyand radiotherapy in patients with locally advanced esophagealcancer: Interim analysis of a phase II trial. J Clin Oncol 14(3):829-837,1996.
18. Bessell JR, DeVitt PG, Gill PG, et al: Prolonged survivalfollows resection of oesophageal SCC downstaged by prior chemoradiotherapy.Aust NZ J Surg 66(4):214-217, 1996.
19. Adelstein DJ, Rice TW, Becker M, et al: Concurrent chemotherapy(CCT), accelerated fractionation radiation (AFR) and surgery foresophageal cancer. Proc Am Soc Clin Oncol 15:203, 1996.
Articles in this issue
over 29 years ago
Antisense Gene Therapy Trials Underway in Patients With CMLover 29 years ago
BOOK REVIEW: Leukemiaover 29 years ago
Most Terminal AIDS Patients Want to Be Revived if Their Heart Stopsover 29 years ago
Disease Management: State of the Art in Pancreatic Cancerover 29 years ago
How to Better Communicate Cancer Risk to Patientsover 29 years ago
Gemcitabine Shows Promise as Combination Agent in NSCLCover 29 years ago
Data Review Shows Fruits and Vegetables Can Block Major CancersNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.