Oncology NEWS International
- Oncology NEWS International Vol 12 No 2
- Volume 12
- Issue 2
ODAC Cites Clinical Benefits of Bexxar, Safety Concerns
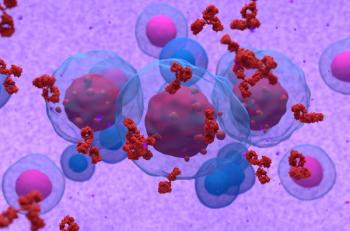
BETHESDA, Maryland-Members of the FDA’s Oncologic Drugs Advisory Committee (ODAC) gave a mixed review to Corixa’s Bexxar (tositumomab and iodine I-131-tositumomab), a radioactive-labeled monoclonal antibody intended to treat certain non-Hodgkin’s lymphoma (NHL) patients.
BETHESDA, MarylandMembers of the FDA’s Oncologic Drugs Advisory Committee (ODAC) gave a mixed review to Corixa’s Bexxar (tositumomab and iodine I-131-tositumomab), a radioactive-labeled monoclonal antibody intended to treat certain non-Hodgkin’s lymphoma (NHL) patients.
The committee agreed that the drug showed evidence of clinical benefit in NHL patients, with unusually high rates of complete remissions (see ONI January 2003, page 1). ODAC voted 10 to 3 in support of the efficacy of Bexxar in rituximab (Rituxan)-refractory patients and unanimously supported its clinical utility in chemotherapy-relapsed and refractory, low-grade NHL, with or without transformation.
ODAC members, however, expressed concern about whether the clinical trial data presented to them clearly demonstrated that the drug’s benefits outweigh its risks, particularly with regard to the occurrence of secondary cancers. FDA did not ask the panel to vote on whether to recommend that FDA approve Bexxar.
Corixa has applied to the FDA for two types of approval for the drug. The company seeks accelerated approval to market the drug as a treatment for patients with relapsed or refractory low-grade or transformed low-grade NHL. Corixa also is seeking standard approval to market Bexxar for the treatment of patients with rituximab-refractory follicular NHL.
During the ODAC meeting, Corixa presented data from two pivotal and three supportive studies to back its new drug application. The five trials showed overall response rates ranging from 46% to 63% and complete response rates ranging from 20% to 33%. Safety data presented by the company from 620 Bexxar-treated patients showed that 14 of them died from myelodysplastic syndrome (MDS) or acute myelogenous leukemia (AML), with an annualized incidence for the two diseases of 2.2% a year.
During the committee’s discussion, chair Donna Przepiorka, MD, PhD, of the University of Tennessee in Memphis, called the complete response rates for Bexxar "amazing in patients who have been so heavily pretreated. However, I am concerned about the hematologic data as well as the potential for leukemia in these patients. This is certainly not something I would jump to as a first-line therapy in patients with stage III or IV disease. But definitely for patients with refractory disease or refractory-relapsed disease, it is better than anything we can do currently." Her remarks seemed to sum up the general views of most of her fellow ODAC members.
Bexxar’s monoclonal antibody targets the CD20 surface antigen, which is expressed on B-cell tumor cells. The antibody is labeled with iodine-131 and when it attaches to the CD20 antigen, the radionuclide delivers a deadly dose of radiation to the cancer cell. Bexxar also has an affinity for a few normal cells.
To support its accelerated request, Corixa presented pivotal data from a phase II trial designated RIT-II-004, which treated 60 patients with chemotherapy-refractory low-grade or transformed low-grade NHL at eight sites. Patients served as their own controls, and the trial’s primary endpoint was the number of patients having a longer duration of response after Bexxar, compared with the number of patients with a longer duration of response after their last qualifying chemotherapy (longer being more than 30 days). Twenty-six patients had a longer duration of response after Bexxar, according to the company’s summary, vs 5 who had a longer response after their last chemotherapy.
Other statistically significant comparisons favoring Bexxar were overall response (47% vs 12%), duration of response (11.7 vs 4.1 months), and complete response (20% vs 2%). Twenty-five percent of the patients were classified as long-term durable responders.
RIT-II-002, a phase II randomized trial of the safety and efficacy of Bexxar vs its unlabeled monoclonal antibody, served to support Corixa’s request for the drug’s standard approval. The study enrolled 78 patients with rituximab-refractory follicular NHL at nine sites.
The company reported a significant difference in the complete remission rate, the study’s primary efficacy endpoint. Fourteen of the 42 Bexxar-treated patients (33%) had a complete remission vs 3 of 36 (8%) of those who received only the antibody. The overall response rate was also significantly higher with Bexxar, 55% vs 19%. Patients were allowed to cross over to Bexxar if their disease progressed. Twenty of the 61 patients who received Bexxar either in the initial randomization or as crossover therapy were classified as long-term durable responders.
Safety Questions
Although largely agreeing with the sponsor’s efficacy findings, the FDA medical review team raised major questions regarding the safety of the drug, particularly the occurrence of secondary malignancies in Bexxar-treated patients. It also expressed concern about significant amounts of missing study data, due, in part, to high withdrawal rates in disease progression or death, and also to a failure to collect data from patients who remained alive for analysis of survival.
The team focused its safety analysis on 229 of the 284 patients in the two pivotal and three supportive studies presented by Corixa. The rest were excluded for several reasons, including 17 patients who received only the monoclonal antibody in Study RIT-II-002.
The FDA team noted that toxicities occurred that were related to both the radioactive iodine and the monoclonal antibody. Those primarily due to the radionuclide included neutropenia (64% of patients), thrombocytopenia (54%), and anemia (19%). Other Bexxar adverse events included infections (43%) and hemorrhagic events (12%).
"The majority of these clinical sequelae of myelosuppression were not serious," the FDA reviewers told ODAC members. "The most common serious adverse events were infections and secondary malignancies." Corixa’s data showed 13 cases of MDS or AML among the 229 patients.
Articles in this issue
about 23 years ago
Some Activity for Gefitinib in Heavily Pretreated Breast Cancerabout 23 years ago
Brachytherapy Results Similar for Blacks, Whitesabout 23 years ago
Dose-Dense Chemo Ups Survival in Node+ Breast Cancerabout 23 years ago
MR Spectroscopy IDs Breast Cancers, Node Involvementabout 23 years ago
ODAC Wants More Data on Expanded Casodex Indicationabout 23 years ago
SuperGen Submits First NDA Module for Pancreatic Cancer Drugabout 23 years ago
Two Added to ONI’s Oncology Nursing Editorial Advisory Boardabout 23 years ago
Bortezomib Active in Relapsed/Refractory Myelomaabout 23 years ago
Telomerase Potential Cancer BiomarkerNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.