- ONCOLOGY Vol 23 No 1
- Volume 23
- Issue 1
A Patient With Metastatic Melanoma of the Small Bowel
Melanoma frequently metastasizes to the small bowel. In this installment of Clinical Quandaries, we describe the case of 74-year-old man who presented with this rare but well described manifestation of malignant melanoma
We report the case of a 74-year-old man with metastatic melanoma of the small bowel. Melanoma metastasizing to the small bowel is a rare but well described presentation of the disease, detected clinically in only 2% to 5% of these patients. Its presentation is similar to other gastrointestinal tract tumors, with symptoms of abdominal pain or anemia prevailing. Recent studies have implicated the chemokine receptor CCR9 and its ligand CCL25 as signals that allow malignant melanoma cells to preferentially metastasize to the small bowel. Common imaging modalities used to detect these small bowel lesions include contrast-enhanced computed tomography (CT) scans and upper gastrointestinal series with small bowel follow-through. Given the low sensitivity of these modalities, newer helical CT scanners, 18F-2-fluoro-2-deoxy-D-glucose–positron emission tomography (FDG PET)/CT, and capsule endoscopy are now being recommended to replace the older imaging techniques. Current treatment modalities include surgical resection, which has been shown to increase overall survival, and adjuvant immunotherapy, whose efficacy is currently being questioned. A review of the current literature describing this rare occurrence is included to compare with our patient's presentation, diagnosis, and management.
Melanoma frequently metastasizes to the small bowel. In this installment of Clinical Quandaries, we describe the case of 74-year-old man who presented with this rare but well described manifestation of malignant melanoma.
Case Report
FIGURE 1
Capsule Endoscopy
A 74-year-old man with a 3-year history of malignant melanoma presented with an episode of lower gastrointestinal (GI) bleeding. He developed progressively worsening anemia and required frequent transfusions (totaling 2 units of packed red blood cells). During an extensive GI workup, he was noted on capsule endoscopy to have one ulcerated and bleeding lesion in the ileum that was not accessible to endoscopic biopsy (
In addition to anemia, the patient described symptoms of anorexia, a 30 lb weight loss over the past 6 months, and weekly episodes of melena. His past medical history includes surgical resection of two separate cutaneous lesions on his back followed by 6 months of interferon-alpha therapy which was stopped due to poor patient tolerance. In the past year, he was noted to have bilateral axillary lymphadenopathy on exam. This was thought to represent metastatic disease, for which he underwent bilateral axillary lymph node dissections. Only one lymph node in each axilla was found to be positive for malignancy, and the patient received no further treatment at that time.
FIGURE 2
FDG-PET
After consultation and review of the current PET imaging, the patient underwent surgical resection of the area of increased uptake in the small bowel with its attached mesentery and lymph nodes. Two abnormal lesions were found in the ileum. The smaller lesion was proximal and appeared to be an intussusception, and the other more distal lesion was a 3- to 4-cm intraluminal mass, nearly circumferential in nature (
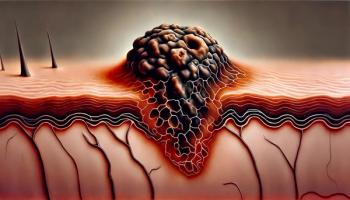
Pathologic review of the resected lesions included immunohistochemical staining with a melanoma cocktail (
Discussion
FIGURE 3
Gross Resection
the small bowel. A large review of autopsies in 1964 at Memorial Sloan-Kettering Cancer Center found that the small bowel was the most common site of metastasis, found in 58% of malignant melanoma patients.[1] Another study, in 1999, also demonstrated that a large proportion of patients (50%) had metastasis to the small bowel.[2] These findings have been confirmed in other autopsy studes.[3] Though it is prevalent, small bowel metastasis has been detected clinically in only 2% to 5% of patients with malignant melanoma.[4] The average time of detection of metastasis after diagnosis of the primary tumor, for all GI tract metastasis, was 43.8 ± 11.3 months.[5] A study by Bender et al in 2001 showed similar results, with the average time from diagnosis to detection at 3.2 years.[6] The most typical symptoms at presentation were anemia or abdominal pains, but can include fatigue, constipation, tenesmus, small bowel obstruction, perforation, intussusception, and hematemesis.[3]
In addition, cases of primary melanoma of the small bowel have been reported. These are not only rare, but often are difficult to distinguish from a primary lesion.[3,7] Suggested clinical criteria for differentiation of primary from metastatic small bowel involvement include lack of concurrent or previous removal of a melanotic lesion, no other organ involvement, in situ change in adjacent GI epithelium, and disease-free survival of 12 months after initial diagnosis.[8] Histologic criteria for primary melanoma of the small bowel include observation of one or more of the following: varying proportions of spindle cells, junctional proliferation within the mucosa, large eosinophilic nuclei, and excess cytoplasm.[7,9] Ultimately, the prognosis for these patients is poor, with a median survival of only 4 to 6 months.[3]
Mechanisms
FIGURE 4
Surgical Pathology
While melanoma is well known to metastasize to the small bowel, the mechanism for this localization is poorly understood. Studies in the past few years, however, have suggested a possible explanation for this metastatic affinity to the small bowel.[11,12] Chemokine receptors are known to be upregulated in certain cancers.[11] A landmark paper in 2001 by Muller and colleagues found that CXCR4 and CCR7 were highly expressed in human breast cancer cells, malignant breast tumors, and breast metastases.[13] The ligands of these receptors, CXCL12/SDF-1α and CCL21/6Ckine, respectively, exhibited increased levels of expression in organs representing the first destination of cancer metastases. CXCR4 serves as a homing signal to distant organs (bone, liver, lung, and lymph node).[14] Others have shown functional expression of CXCR4 acting in the same capacity in colorectal carcinoma with its preference to metastasize to the liver.[11]
Takeuchi et al further elucidated the ability of melanoma metastases to spread to specific organs.[15] They showed that CCL21/SLC (the ligand for CCR7) promoted the migration of melanoma cells and may in fact be the mechanism for the recruitment and directing of melanoma cells to the sentinel node. They also noted that CCR7 expression significantly correlated with Breslow thickness, suggesting its potential to be used as a prognostic indicator.[11] Furthermore, CCL25, a ligand of CCR9, is expressed predominantly in the thymus and on the epithelium of the small intestine and selectively in small intestine infiltrating T cells.[11] Increased numbers of circulating CCR9-positive lymphocytes have even been found in patients with inflammatory bowel disease.[11]
These studies produced the basis for investigating the CCR9-CCL25 axis for its role in the site-specific metastasis of melanoma to the small bowel.[11] This group also showed CCR9 overexpression in 88 of 102 paraffin-embedded metastatic melanomas from the small intestine. Expression was noted in all samples from small bowel derived melanoma metastases and in 0 of 96 samples from metastatic melanomas derived from other sites. In addition, they demonstrated tumor migration in response to CCL25 and inhibition of that migration via anti-CCR9 antibodies or small interfering RNA (siRNA).[11]
Another group found that CCR9 was highly expressed on all melanoma cells, all melanoma cell lines isolated from small bowel metastases, and on a proportion of other cell lines.[12] However, they noted that only the melanoma cell lines from small bowel metastases were responsive to the CCR9 ligand, further strengthening the tie between its site-specific metastatic ability and CCR9.
Detection
Imaging modalities commonly used to detect metastatic lesions in the small intestine are contrast-enhanced computed tomography (CT) and upper gastrointestinal series with small bowel follow-through. The typical finding that invokes consideration for metastatic melanoma is a discrete polypoid mass with central ulceration that is described as a target or bulls-eye lesion.
A review of these typicallesions demonstrated that they were actually fairly uncommon, being observed in only 9% of the scans reviewed.[6] Additionally, the two modalities had a poor sensitivity for detection of these lesions (58% and 66%, respectively), and were determined to be unreliable for adequate preoperative assessment.[6] Another study found similar results, with CT having a sensitivity of only 46.7% for detection of this disease in the bowel.[10] This low detection rate may be related in part to the poor outcomes seen with this disease compared with gastric and colonic metastases.[16]
Accordingly, several authors are now proposing new imaging modalities for this disease process. Volume-challenged imaging of the small bowel with newer helical CT algorithms are being studied, while others note that FDG-PET/CT is a reliable method for detection with sensitivity superior to conventional CT imaging methods and FDG-PET alone.[6,17] Recently, Albert and colleagues were able to localize a melanoma metastasis with capsule endoscopy and recommend its use in combination with CT for detection of these lesions.[16]
Treatment and Survival
The current treatment of choice for metastatic small bowel lesions in melanoma is surgical resection. Ollila et al found that symptomatic patients derived a significant benefit from surgical resection.[18] The median survival for patients who underwent curative resection was 48.9 months, compared to 5.4 and 5.7 months for palliative and nonsurgical interventions, respectively, with only 1 operative death (1.4%) and 1 major operative complication (1.4%) out of 69 patients treated. They also found that intestinal tract metastases, especially when these are the primary site of distant metastasis, were the only prognostic indicators for survival. Agrawal et al found a greater median survival in patients with complete surgical resection (14.9 months) vs patients with residual disease (6.9 months) and in patients with serum lactate dehydrogenase (LDH) < 200 U/L (13.6 months) vs LDH 200 (6.5 months).[19] This study also demonstrated a low morbidity and mortality 8.8% and 2.9%, respectively.
Berger and colleagues compared outcomes in patients who had not had surgical treatment with those undergoing partial or complete resection. Patients with metastatic disease who were not treated surgically had a mean survival of only 4.1 months, whereas those having a partial resection had a survival of 8.9 months, and those who were completely resected demonstrated the greatest survival at 23.5 months.[20]
Another study, by Gutman et al in 2001, showed similar benefits in patients who were treated surgically vs medically for gastrointestinal tract metastases.[21] The surgery group had a median survival of 11 months, whereas the medically treated groups median survival was 5 months. This same study found similar results in patients undergoing a secondary procedure. Those who had a second surgical procedure had a 5-month greater survival than the nonsurgical intervention group (14 vs 9 months). In 2007, Hodgson et al echoed the fact that patients who underwent curative resection had greater survival than those who underwent palliative resection.[22] Interestingly, they found that serum albumin levels over 3.5 g/L significantly correlated with increased survival. There has also been debate as to the efficacy of surgical resection on minimally symptomatic or asymptomatic patients. Gutman and colleagues found that the severity of symptoms did not correlate with survival in their series.[21] In another series, Hodgson was unable to show a survival benefit in completely asymptomatic patients.[22] Although these groups did not show any survival benefit in patients with minimal or no symptoms, larger series are needed to provide a more definitive answer for the role of surgical resection in this subset of patients.
Adjuvant Therapy
Adjuvant therapies for metastatic melanoma have recently come under scrutiny. Several large centers have moved away from chemotherapy and radiotherapy in exchange for immunotherapy.[22] Unrandomized phase II trials have demonstrated a modest benefit in select patients, but no increase in overall survival has been demonstrated in any randomized controlled trials.[9]
A recent report by Berger and colleagues found no survival benefit with immunotherapy using interleukin-2 (Proleukin). This lack of survival benefit was also reported by Agrawal et al, whose immunotherapy-treated group had a 7.3-month median survival vs a 7.8-month survival for untreated patients.[19,20] However, it should be noted that both of these studies were small series, underpowered to make any definitive statement about the effectiveness of immunotherapy on survival.
A trial by the Eastern Cooperative Oncology Group (ECOG 1684) found an increase in survival for stage IV melanoma using high-dose interferon alfa-2b (Intron A) at 2.3 to 3.8 years of follow-up, only to find that this advantage was lost at the 10-year follow-up.[23] A larger confirmatory trial from the same group (ECOG 1690) again found no long-term benefit on survival.[23]
Conclusions
In conclusion, melanoma patients presenting with GI symptoms should be evaluated to rule out small bowel metastases. New investigations of cytokine receptors and their ligands, especially CCR9, have suggested a mechanism to explain how melanoma can preferentially metastasize to the small bowel and may hold value for future diagnostic and prognostic advances in this disease.
Localization of these tumors in the small bowel can be a challenging problem, and future studies will focus on imaging modalities with improved sensitivity and resolution over conventional techniques for detection of these lesions. This is important for optimal survival since identification of these lesions allows for better surgical removal, which has been shown to improve overall survival with low morbidity.
Finally, the role of adjuvant therapy is continually evolving, as new drugs are being discovered each year. While the role of immunotherapy is not completely defined for melanoma metastatic to the bowel, ongoing trials with long-term follow-up will determine the optimal adjuvant treatment for patients with this disease.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Dasgupta TK, Brasfield RD: Metastatic melanoma of the gastrointestinal tract. Arch Surg 88:969-973, 1964.
2. Blecker D, Abraham S, Furth EE, et al: Melanoma in the gastrointestinal tract. Am J Gastroenterol 94:3427-3433, 1999.
3. Schuchter LM, Green R, Fraker D: Primary and metastatic diseases in malignant melanoma of the gastrointestinal tract. Curr Opin Oncol 12:181-185, 2000.
4. Gatsoulis N, Roukounakis N, Kafetzis I, et al: Small bowel intussusception due to metastatic malignant melanoma. A case report. Tech Coloproctol 8(suppl 1):141-143, 2004.
5. Wysocki WM, Komorowski AL, Darasz Z: Gastrointestinal metastases from malignant melanoma: Report of a case. Surg Today 34:542-546, 2004.
6. Bender GN, Maglinte DD, McLarney JH, et al: Malignant melanoma: Patterns of metastasis to the small bowel, reliability of imaging studies, and clinical relevance. Am J Gastroenterol 96:2392-2400, 2001.
7. Guraya SY, Al Naami M, Al Tuwaijri T, et al: Malignant melanoma of the small bowel with unknown primary: A case report. J Ayub Med Coll Abbottabad 19:63-65, 2007.
8. Manouras A, Genetzakis M, Lagoudianakis E, et al: Malignant gastrointestinal melanomas of unknown origin: Should it be considered primary? World J Gastroenterol 13:4027-4029, 2007.
9. Liang KV, Sanderson SO, Nowakowski GS, et al: Metastatic malignant melanoma of the gastrointestinal tract. Mayo Clin Proc 81:511-516, 2006.
10. Panagiotou I, Brountzos EN, Bafaloukos D, et al: Malignant melanoma metastatic to the gastrointestinal tract. Melanoma Res 12:169-173, 2002.
11. Amersi FF, Terando AM, Goto Y, et al: Activation of CCR9/CCL25 in Cutaneous melanoma mediates preferential metastasis to the small intestine. Clin Cancer Res 14:638-645, 2008.
12. Letsch A, Keilholz U, Schadendorf D, et al: Functional CCR9 expression is associated with small intestinal metastasis. J Invest Dermatol 122:685-690, 2004.
13. Müller A, Homey B, Soto H, et al: Involvement of chemokine receptors in breast cancer metastasis. Nature 410:50-56, 2001.
14. Richmond A: CCR9 homes metastatic melanoma cells to the small bowel. Clin Cancer Res 14:621-623, 2008.
15. Takeuchi H, Fujimoto A, Tanaka M, et al: CCL21 chemokine regulates chemokine receptor CCR7 bearing malignant melanoma cells. Clin Cancer Res 10:2351-2358, 2004.
16. Albert JG, Gimm O, Stock K, et al: Small-bowel endoscopy is crucial for diagnosis of melanoma metastases to the small bowel: A case of metachronous small-bowel metastases and review of the literature. Melanoma Res 17:335-338, 2007.
17. Strobel K, Skalsky J, Hany TF, et al: Small bowel invagination caused by intestinal melanoma metastasis: Unsuspected diagnosis by FDG-PET/CT imaging. Clin Nucl Med 32:213-214, 2007.
18. Ollila DW, Essner R, Wanek LA, et al: Surgical resection for melanoma metastatic to the gastrointestinal tract. Arch Surg 131:975-980, 1996.
19. Agrawal S, Yao TJ, Coit DG: Surgery for melanoma metastatic to the gastrointestinal tract. Ann Surg Oncol 6:336-344, 1999.
20. Berger AC, Buell JF, Venzon D, et al: Management of symptomatic malignant melanoma of the gastrointestinal tract. Ann Surg Oncol 6:155-160, 1999.
21. Gutman H, Hess KR, Kokotsakis JA, et al: Surgery for abdominal metastases of cutaneous melanoma. World J Surg 25:750-758, 2001.
22. Hodgson R, Fink MA, Jones RM: The role of abdominal resectional surgery in metastatic melanoma. ANZ J Surg 77:855-859, 2007.
23. Hersey P: Adjuvant therapy for high-risk primary and resected metastatic melanoma. Intern Med J 33:33-43, 2003.
Articles in this issue
about 17 years ago
Controversies in the Surgical Management of GIST in the Era of Imatinibabout 17 years ago
Perioperative Treatment of Gastrointestinal Stromal TumorsNewsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.