RADIANT-4: Everolimus Effective in Lung, GI NETs
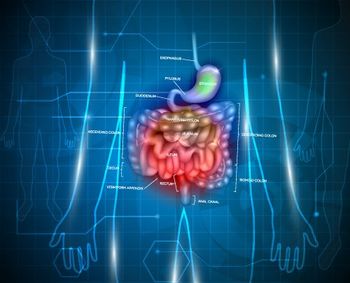
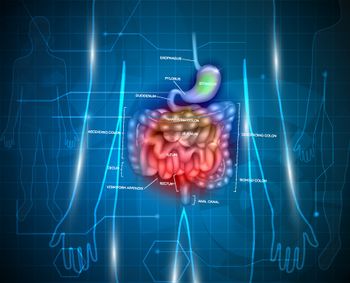
Nonfunctional neuroendocrine tumors of lung or gastrointestinal origin were safely and effectively treated with the mTOR inhibitor everolimus.
Nonfunctional neuroendocrine tumors (NETs) of the lung or of gastrointestinal origin were safely and effectively treated with the mTOR inhibitor everolimus, according to the results of the phase III, placebo-controlled, double-blind RADIANT-4 trial. Treatment with everolimus resulted in a 7.1-month improvement in progression-free survival compared with placebo.
These results (abstract LBA 5) were presented at the 2015 European Cancer Congress (ECC) by James C. Yao, MD, chair of the department of gastrointestinal medical oncology at the University of Texas MD Anderson Cancer Center.
“About 80% of all NETs are thought to be nonfunctional, so, unfortunately, late diagnosis is common and poses a major problem for these patients,” Yao said in a prepared statement. “Although we knew from previous studies that everolimus could delay the growth of pancreatic NETs, this is the first time we have been able to conclusively show that it is effective in other NET sites.”
The study included 302 patients with advanced and progressive NETs of lung/gastrointestinal origin recruited from 13 European countries. The patients were randomly assigned 2:1 to everolimus 10 mg per day plus best supportive care (n = 205) or placebo plus best supportive care (n = 97). The primary endpoint of the study was progression-free survival.
Both groups were well balanced in terms of prior treatments. In the everolimus group, 53% had had prior therapy with a somatostatin analogue (SSA), chemotherapy (26%), and radiotherapy (22%). In the placebo groups, 56% had prior therapy with an SSA, 24% had chemotherapy, and 20% had radiotherapy.
At follow-up, there was a 52% reduction in the relative risk for progression or death in patients assigned to everolimus compared with placebo (hazard ratio [HR], 0.48 [95% confidence interval (CI), 0.28–0.54]; P < .001). The median progression-free survival evaluated by central review was 11 months for everolimus compared with 3.9 months for the placebo arm. The investigator-assessed progression-free survival was similar.
There was an overall response rate of 2% for everolimus compared with 1% for placebo. In addition, the disease control rate was 82% for patients assigned everolimus compared with 65% for those given placebo.
Yao and colleagues also conducted an interim analysis of overall survival that showed a 36% improvement in favor of everolimus (HR, 0.64 [95% CI, 0.40–1.05]; P = .037). However, this difference did not reach statistical significance with the threshold P value for significance being 0.000213; however, Yao noted that “the overall survival analysis is an interim one, and it is too early to be able to be more definite about this at this time.”
Adverse events were mostly grade 1 or 2. For patients assigned everolimus compared with placebo, the most common grade 3/4 adverse events were diarrhea (9% vs 2%), stomatitis (7% vs 0%), abdominal pain (5% vs 5%), and anemia (5% vs 2%).
Newsletter
Stay up to date on recent advances in the multidisciplinary approach to cancer.